What Causes Migraine and Chronic Migraine?
Blue indicates link
Migraine headaches are a bit of a mystery. Researchers have identified possible causes, but they don’t have a definitive explanation. Potential theories include:
- An underlying central nervous disorder may set off a migraine episode when triggered.
- Irregularities in the brain’s blood vessel system, or vascular system, may cause migraines.
- A genetic predisposition may cause migraines
- Abnormalities of brain chemicals and nerve pathways may cause migraine episodes.
What Causes A Migraine
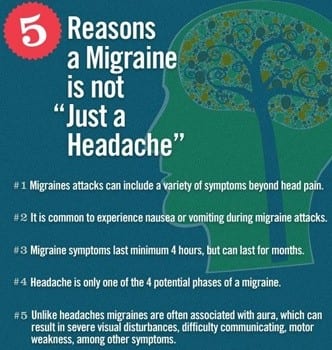
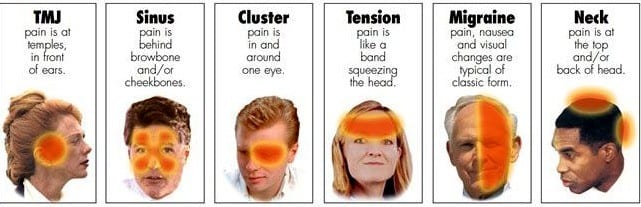
A migraine can cause severe throbbing pain or a pulsing sensation, usually on one side of the head. It’s often accompanied by nausea, vomiting, and extreme sensitivity to light and sound. Migraine attacks can last for hours to days, and the pain can be so severe that it interferes with your daily activities.
For some people, a warning symptom known as an aura occurs before or with a headache. An aura can include visual disturbances, such as flashes of light or blind spots, or other disturbances, such as tingling on one side of the face or in an arm or leg and difficulty speaking.
Medications can help prevent some migraines and make them less painful. The right medicines, combined with self-help remedies and lifestyle changes, might help.
Migraines, which often begin in childhood, adolescence, or early adulthood, can progress through four stages: prodrome, aura, attack, and post-drome. Not everyone who has migraines goes through all stages.
The Stages of A Migraine:
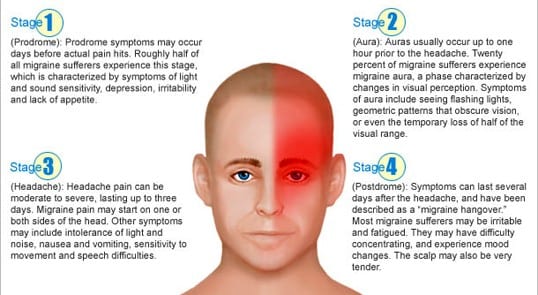
Prodrome:
One or two days before a migraine, you might notice subtle changes that warn of an upcoming migraine:
Constipation
Mood changes,
Depression to euphoria
Food cravings
Neck stiffness
Increased thirst and urination Frequent yawning
Aura:
For some people, aura might occur before or during migraines. Auras are reversible symptoms of the nervous system. They’re usually visual but can also include other disturbances. Each symptom usually begins gradually, builds up over several minutes, and lasts for 20 to 60 minutes.
Examples of migraine aura include:
Visual phenomena, such as seeing various shapes, bright spots, or flashes of light
Vision loss
Pins and needles sensations in an arm or leg
Weakness or numbness in the face or one side of the body
Difficulty speaking
Hearing noises or music
Uncontrollable jerking or other movements
Attack:
A migraine usually lasts from four to 72 hours if untreated. How often migraines occur varies from person to person. Migraines might occur rarely or strike several times a month.
During a migraine, you might have:
Paragraph Pain usually on one side of your head, but often on both sides
Pain that throbs or pulses
Sensitivity to light, sound, and sometimes smell and touch
Nausea and vomiting
Post-drome:
After a migraine attack, you might feel drained, confused, and washed out for up to a day. Some people report feeling elated. The sudden head movement might bring on the pain again briefly.
Though migraine causes aren’t fully understood, genetics and environmental factors appear to play a role.
Changes in the brainstem and its interactions with the trigeminal nerve, a major pain pathway, might be involved. So might imbalances in brain chemicals — including serotonin, which helps regulate pain in your nervous system.
Researchers are studying the role of serotonin in migraines. Other neurotransmitters play a role in the pain of migraines, including calcitonin gene-related peptide (CGRP).
Migraine triggers. There are a number of migraine triggers, including:
Hormonal changes in women. Fluctuations in estrogen, such as before or during menstrual periods, pregnancy, and menopause, seem to trigger headaches in many women.
Hormonal medications, such as oral contraceptives and hormone replacement therapy, also can worsen migraines. Some women, however, find their migraines occurring less often when taking these medications.
Drinks.
These include alcohol, especially wine, and too much caffeine, such as coffee.
Stress. Stress at work or home can cause migraines.
Sensory stimuli. Bright lights and sun glare can induce migraines, as can loud sounds. Strong smells — including perfume, paint thinner, secondhand smoke, and others — trigger migraines in some people.
Sleep changes. Missing sleep, getting too much sleep, or jet lag can trigger migraines in some people.
Physical factors. Intense physical exertion, including sexual activity, might provoke migraines.
Weather changes. A change of weather or barometric pressure can prompt a migraine.
Medications. Oral contraceptives and vasodilators, such as nitroglycerin, can aggravate migraines.
Foods. Aged cheeses and salty and processed foods might trigger migraines. So might skip meals or fasting.
Food additives. These include the sweetener aspartame and the preservative monosodium glutamate (MSG), found in many foods.
What can trigger a migraine:
Unfortunately, scientists have yet to identify a cause. The best way to avoid migraines is to avoid what starts them in the first place. A migraine trigger is unique to each person, and it’s not uncommon for a person to have several migraine triggers.
The most common migraine triggers include:
Food
Salty foods or aged foods, such as cheese and salami, may cause migraine headaches. Highly processed foods can also trigger a migraine.
Skipping meals
People with a history of migraines shouldn’t skip meals or fast unless it’s done under a doctor’s supervision.
Drink
Alcohol and caffeine may cause these headaches.
Preservatives and sweeteners
Some artificial sweeteners, such as aspartame, can trigger a migraine. The popular preservative monosodium glutamate (MSG) can, as well. Read labels to avoid them.
Sensory stimulation
Unusually bright lights, loud noises, or strong smells, may set off a migraine headache; flashlights, bright sun, perfume, paint, and cigarette smoke, are all common triggers.
Hormonal changes
Hormone shifts are a common migraine trigger for women. Many women report developing migraine headaches right before or even during their period. Others report hormone-induced migraines during pregnancy or menopause. That’s because estrogen levels change during this time and can trigger a migraine episode.
Hormone medications
Medications, such as birth control and hormone replacement therapies, can trigger or worsen a migraine. However, in some cases, these medicines can actually reduce a woman’s migraine headaches.
Other medications
Vasodilators, such as nitroglycerin, can trigger a migraine.
Physical stress
Extreme exercise, physical exertion, and even sexual activity can trigger migraine headaches.
Sleep cycle changes
If you’re not getting regular, routine sleep, you may experience more migraines. Don’t bother trying to “make up” for lost sleep on the weekends, either. Too much sleep is just as likely to cause a headache as too little.
Weather changes
What Mother Nature is doing outside may affect how you feel on the inside. Changes in weather and shifts in barometric pressure can trigger a migraine.
Factors that increase your risk for migraines
Not everyone exposed to migraine triggers will develop a headache. However, some people are more sensitive to them. Several risk factors can help predict who is more prone to having migraine headaches.
These risk factors include:
Age
Migraines can first appear at any age. However, most people will experience their first migraine during adolescence. According to the Mayo Clinic, migraines usually improve after age 30.
Family history
If a close family member has migraines, you’re more likely to have them. In fact, 90 percent of migraine patients have a family history of migraines. Parents are the best predictor of your risk. If one or both of your parents have a history of migraines, your risk is higher.
Gender
During childhood, boys experience migraine headaches more than girls. After puberty, however, women are three times more likely to have migraines than men.
Talk to your doctor
Make an appointment with your doctor if you are having migraines. They can diagnose the underlying condition if there is one, and prescribe treatments. Your doctor can also help you determine what lifestyle changes you need to make to manage your symptoms.
Diagnosis
If you have migraines or a family history of migraines, a doctor trained in treating headaches (neurologist) will likely diagnose migraines based on your medical history, symptoms, and a physical and neurological examination.
If your condition is unusual, complex, or suddenly becomes severe, tests to rule out other causes for your pain might include:
MRI. An MRI scan uses a powerful magnetic field and radio waves to produce detailed images of the brain and blood vessels. MRI scans help doctors diagnose tumors, strokes, bleeding in the brain, infections, and other brain and nervous system (neurological) conditions.
CT scan. A CT scan uses a series of X-rays to create detailed cross-sectional images of the brain. This helps doctors diagnose tumors, infections, brain damage, bleeding in the brain, and other possible medical problems that may be causing headaches.
Treatment
Migraine treatment is aimed at stopping symptoms and preventing future attacks.
Many medications have been designed to treat migraines. Medications used to combat migraines fall into two broad categories:
Pain-relieving medications. Also known as an acute or abortive treatment, these types of drugs are taken during migraine attacks and are designed to stop symptoms.
Preventive medications. These types of drugs are taken regularly, often daily, to reduce the severity or frequency of migraines.
Your treatment choices depend on the frequency and severity of your headaches, whether you have nausea and vomiting with your headaches, how disabling your headaches are, and other medical conditions you have.
Medications for relief
Medications used to relieve migraine pain work best when taken at the first sign of an oncoming migraine — as soon as signs and symptoms of a migraine begin.
Medications that can be used to treat it include:
Pain relievers. These over-the-counter or prescription pain relievers include aspirin or ibuprofen (Advil, Motrin IB, others). When taken too long, these might cause medication-overuse headaches, and possibly ulcers and bleeding in the gastrointestinal tract.
Migraine relief medications that combine caffeine, aspirin, and acetaminophen (Excedrin Migraine) may be helpful, but usually only against mild migraine pain. Triptans.
These are prescription drugs such as sumatriptan (Imitrex, Tosymra) and rizatriptan (Maxalt) are prescription drugs used for migraine because they block pain pathways in the brain. Taken as pills, shots, or nasal sprays, they can relieve many symptoms of migraine. They might not be safe for those at risk of a stroke or heart attack.
Dihydroergotamines (D.H.E. 45, Migranal). Available as a nasal spray or injection, these are most effective when taken shortly after the start of migraine symptoms for migraines that tend to last longer than 24 hours. Side effects can include the worsening of migraine-related vomiting and nausea.
People with coronary artery disease, high blood pressure, or kidney or liver disease should avoid dihydroergotamines. This new oral tablet is approved for the treatment of migraine with or without aura. In drug trials, lasmiditan significantly improved pain as well as nausea and sensitivity to light and sound.
Lasmiditan can have a sedative effect and cause dizziness, so people taking it are advised not to drive or operate machinery for at least eight hours. Lasmiditan also shouldn’t be taken with alcohol or other drugs that depress the central nervous system.
This oral calcitonin gene-related peptide receptor antagonist is approved for the treatment of acute migraine with or without aura in adults. It’s the first drug of this type approved for migraine treatment.
In drug trials, ubrogepant was more effective than a placebo in relieving pain and other migraine symptoms such as nausea and sensitivity to light and sound two hours after taking it. Common side effects include dry mouth, nausea, and excessive sleepiness. Ubrogepant should not be taken with strong CYP3A4 inhibitor drugs.
Opioid medications.
For people who have migraines and can’t take other migraine medications, narcotic opioid medications, especially those that contain codeine, might help. Because they can be highly addictive, these are usually used only if no other treatments are effective.
Anti-nausea drugs. These can help if your migraine with aura is accompanied by nausea and vomiting. Anti-nausea drugs include chlorpromazine, metoclopramide (Reglan), or prochlorperazine (Compro). These are usually taken with pain medications.
Preventive medications
Medications can help prevent frequent migraines. Your doctor might recommend preventive medications if you have frequent, long-lasting, or severe headaches that don’t respond well to treatment.
Preventive medication is aimed at reducing how often you get a migraine how severe the attacks are and how long they last.
Options include:
Blood pressure-lowering medications. These include beta-blockers such as propranolol (Inderal, Innopran XL, and others) and metoprolol tartrate (Lopressor). Calcium channel blockers such as verapamil (Tarka, Verelan) can be helpful in preventing migraines with aura.
Antidepressants.
A tricyclic antidepressant (amitriptyline) can prevent migraines. Because of the side effects of amitriptyline, such as sleepiness and weight gain, other antidepressants might be prescribed instead.
Anti-seizure drugs. Valproate and topiramate (Topamax) might help you have less frequent migraines but can cause side effects such as dizziness, weight changes, nausea, and more.
Botox injections. Injections of onabotulinumtoxinA (Botox) about every 12 weeks help prevent migraines in some adults.
Lifestyle and home remedies:
When symptoms of migraine start, try heading to a quiet, darkened room. Close your eyes and rest or take a nap. Place a cool cloth or ice pack wrapped in a towel or cloth on your forehead or at the back of your neck.
Other practices that might soothe migraine with aura pain include:
Try relaxation techniques. Biofeedback and other forms of relaxation training teach you ways to deal with stressful situations, which might help reduce the number of migraines you have.
Develop a sleeping and eating routine. Don’t sleep too much or too little. Set and follow a consistent sleep and wake schedule daily. Try to eat meals at the same time every day.
Drink plenty of fluids. Staying hydrated, particularly with water, might help.
Keep a headache diary. Continue recording in your headache diary even after you see your doctor. It will help you learn more about what triggers your migraines and what treatment is most effective.
Exercise regularly. Regular aerobic exercise reduces tension and can help prevent a migraine. If your doctor agrees, choose an aerobic activity you enjoy, such as walking, swimming, and cycling. Warm up slowly, however, because sudden, intense exercise can cause headaches.
Regular exercise can also help you lose weight or maintain a healthy body weight, and obesity is thought to be a factor in migraines.
Alternative Remedies For Treating Migraines
Nontraditional therapies might help with chronic migraine pain.
Acupuncture. Clinical trials have found that acupuncture
Acupuncture. Clinical trials have found that acupuncture may be helpful for headache pain. In this treatment, a practitioner inserts many thin, disposable needles into several areas of your skin at defined points. Biofeedback. Biofeedback appears to be effective in relieving migraine pain. This relaxation technique uses special equipment to teach you how to monitor and control certain physical responses related to stress, such as muscle tension.
Cognitive-behavioral therapy.
Cognitive-behavioral therapy may benefit some people with migraines. This type of psychotherapy teaches you how behaviors and thoughts affect how you perceive pain.
Herbs, vitamins, and minerals.
There is some evidence that the herbs feverfew and butterbur might prevent migraines or reduce their severity, though study results are mixed. Butterbur isn’t recommended because of safety concerns.
A high dose of riboflavin (vitamin B-2) may also prevent migraines or reduce the frequency of headaches. Coenzyme Q10 supplements might decrease the frequency of migraines, but larger studies are needed.
Due to low magnesium levels in some people with migraines, magnesium supplements have been used to treat migraines, but with mixed results.
Yoga or stretching:
Yoga is thought to help improve blood flow and reduce muscle tension, which can help relieve symptoms for people who get migraines.
A comprehensive 2014 study compared conventional migraine treatment with and without the addition of regular yoga practice.
The researchers found that the group who participated in a yoga program had greater relief than the group who joined in conventional treatment alone.
Herbal Remedies For Treating Migraines
Essential oils
Essential oils are often used as natural remedies or as an antimicrobial in homemade cleaning products.
Lavender is an essential oil often recommended as a remedy for stress, anxiety, and headaches. Another small study published in European Neurology found that lavender oil inhalation helped reduce the severity of migraine headaches in some people.
First used in ancient Greece as early as the fifth century B.C., feverfew (or “feather few”) has been used to treat a variety of ailments. These include fever, swelling, and inflammation. People commonly took the herb to relieve aches and pains such as headaches in the first century.
The plant is native to the Balkan Mountains but can now be found nearly worldwide. Eastern European cultures traditionally used feverfew for headaches, insect bites, and other pain. More modern uses have extended to the treatment of:
- migraines
- dizziness
- inflammation
- breathing problems
Feverfew is usually prepared by drying the leaves, flowers, and stems. This combination is also used to make supplements and extracts. Some cultures eat the leaves raw.
A 2011 review suggests that feverfew is an effective treatment for migraines, fever, the common cold, and arthritis. However, a Cochrane review of five large clinical trials showed little to no benefit for the majority of people who experience migraines.
Feverfew may cause minor side effects such as bloating, canker sores, and nausea. You may also experience moderate side effects when discontinuing use. These side effects can include difficulty sleeping, increased headaches, and joint pain.
Pregnant women, people taking blood-thinning medications, and people with allergies to the daisy family should avoid the use of feverfew.
Butterbur is found in wet, marshy areas of Europe, Asia, and North America. People once used the leaves of the plant to wrap and preserve butter during warm weather, which is how butterbur got its name. It’s been used throughout history for a variety of purposes. The Greek physician Dioscurides originally used the plant as a skin ulcer remedy. Since then, it’s been used to treat:
- headaches
- asthma
- allergies
- cough
- fever
- gastrointestinal problems
- general pain
Most butterbur herbal remedies use its purified root extract, Petasites, in pill form to treat headaches and migraines. A 2012 study published in Neurology supports conclusions from older studies that Petasites is effective for migraine prevention when taken in 50- to 75-milligram doses twice daily.
If you live in Europe, Butterbur might be hard for you to obtain — the U.K. and Germany have both banned butterbur from being sold because of safety concerns with the leading manufacturers.
- spasms
- toothaches
- gastrointestinal problems
- nausea
Peppermint oil and its active ingredient, menthol, is available in liquid capsule form. Tea versions are also available for easy brewing.
A 2010 study published in the International Journal of Clinical Practice found that menthol was effective at stopping migraine pain and easing nausea when applied to the forehead and temples in a 10 percent solution.
Research is limited on its clinical effectiveness, but topical peppermint oil may be a good herbal option for the relief of migraine pain. Peppermint oil is one of the easiest herbal remedies to try because of its prevalence in health food stores and pharmacies.
Willow bark extract (WBE) was used in the development of aspirin, a well-known over-the-counter pain reliever, fever reducer, and anti-inflammatory drug. WBE contains an anti-inflammatory ingredient called salicin. A 2012 study suggests WBE is also an effective antioxidant.
Willow is a tree found in Europe, Asia, and North America. It’s been used since the time of Hippocrates (400 B.C.) when people would chew the bark for its anti-inflammatory and fever-relieving effects. Willow was later used in China and Europe for headaches, osteoarthritis, tendonitis, and lower back pain.
Willow bark can be found in capsule form and as a chewable bark at most health food stores.
Ginger is a tropical Asian plant. It’s been used in herbal medicines in China for over 2,000 years. It’s also been popular in Indian and Arabic medicines since ancient times. Ginger has traditionally been used as a remedy for:
- headaches
- stomach pain
- nausea
- arthritis
- Cold and flu symptoms
- neurological problems
Ginger has been well-documented as anti-inflammatory, antiviral, antifungal, and antibacterial. In addition, a 2014 study published in the Phytotherapy Research showed that ginger powder’s benefits were comparable to sumatriptan’s, a common prescription migraine drug, but with fewer side effects.
Most people can tolerate fresh or dried ginger root, supplements, or extract. Be careful not to combine ginger supplements with blood thinners because of potential drug interactions.
Ginger capsules and ginger tea are both relatively easy to obtain in almost any grocery store or pharmacy. You can also try drinking ginger water.
Caffeinated teas became common in China during the Ming Dynasty. They exploded in popularity in Europe during the 18th and 19th centuries. Green tea was used in combination with other herbs for migraine pain in traditional Chinese medicine. Coffee initially gained recognition in Arabia. Yerba mate, a less widely known caffeinated tea, originated in South America.
People in many cultures primarily consumed caffeine to help treat:
- headaches
- high blood pressure
- stomach problems
- sexually transmitted diseases
- cancer
- circulatory problems
- inflammation
- skin damage
- kidney disease
Caffeine is also found in many over-the-counter pain relievers today.
Although caffeine is frequently studied in combination with other pain relievers, it’s considered a useful and safe additive in pills for many people who experience migraines. A 2012 study found that a combination of 1,000 milligrams (mg) of acetaminophen and 130 mg of caffeine is particularly helpful. However, caffeine withdrawal and caffeine intake can also be triggers for headaches and migraines.
Valerian is native to Europe and Asia. It’s now also commonly found in North America. The use of valerian traces back to ancient Greece and Rome from the time of Hippocrates. It was recognized as a remedy for insomnia a few centuries later. Valerian was known as “all-heal” in the 1500s, as it was used to treat a multitude of ailments. These included:
- insomnia
- headaches
- heart palpitations
- tremors
- anxiety
It’s sometimes used in the modern treatment of headaches, but valerian hasn’t been researched enough to determine its usefulness in the treatment of migraine pain.
Valerian is usually taken as a supplement, tea, or tincture made from dried roots. The liquid extract is also available in capsule form. Valerian root capsules are widely sold in the United States.
For over 7,000 years, people across cultures have used coriander seed’s healing and seasoning properties. Coriander was lauded for its ability to treat ailments that ranged from allergies to diabetes to migraines. Traditional Ayurvedic medicine uses coriander to relieve sinus pressure and headaches by pouring hot water over the fresh seeds and inhaling the steam.
Research on the seed’s medicinal effects is generally focused on its potential to treat arthritis and diabetes. More studies need to be conducted to determine if it’s useful as a remedy for migraine pain. However, coriander seed’s anti-inflammatory potential may prove beneficial for some people with migraines.
Coriander seeds can be chewed and used in food or teas. Oral extracts are also available.
Hailing from the same family as carrots, parsley, and celery, dong Quai root has been used as a spice, tonic, and medicinal cream for more than 1,000 years, especially in Japanese, Chinese, and Korean practices. Modern users often mix it with other herbs to treat:
- headaches
- fatigue
- inflammation
- nerve pain
Despite its history, the root hasn’t been studied enough to recommend it as an effective treatment for migraine pain.
Lavender oil was used in ancient Egypt during the mummification process.
Because of its antimicrobial properties and clean scent, it was later added to baths in Rome, Greece, and Persia. The aromatic flowers and their oil were used to treat everything from headaches and insomnia to mental health complaints such as stress and fatigue. Many of these historical uses remain popular today.
A 2012 study suggests that inhaling lavender oil during a migraine may help relieve symptoms quickly. To use lavender oil, breathe in the oil, or apply a diluted solution to the temples. If you don’t dilute it properly, the oil may irritate the skin at the application site. Lavender oil can be toxic when taken orally at certain doses.
- Muscle and joint pain
- memory problems
- concentration difficulties
- nervous disorders
- circulatory problems
- liver ailments
- migraines
Rosemary oil can be diluted and applied topically or inhaled for aromatherapeutic purposes. The plant’s leaves can be dried and ground for use in capsules. It can also be used in teas, tinctures, and liquid extracts. Rosemary is believed to have antimicrobial, antispasmodic, and antioxidant effects. Still, its ability to reduce migraine pain hasn’t been well studied.
Linden, also known as a lime tree or Tilia is a tree whose blossoms have been used in medicinal teas in European and Native American cultures. The plant has been used to calm nerves and ease anxiety, tension, and inflammatory problems, among other issues. The blossoms can also be used in tinctures, liquid extracts, and capsules.
Linden has been shown to have sweat-inducing and sedative properties. It’s been used to relieve tension and sinus headaches, calm the mind, and induce sleep. The flowers have also been used to relieve nasal congestion and lower high blood pressure.
This tea is sometimes used in modern alternative medicine for the treatment of headaches and migraines. There currently isn’t enough research about the effect of linden tea on migraines to recommend it as an effective natural remedy.
The potato has been used in European folk medicine for over 200 years. Country folk medicine has anecdotally supported the use of thick slices of raw potato in calming migraine pain. Traditionally, the slices are cloaked in a thin cloth and wrapped around the head or rubbed directly on the temples to ease tension and pain. There is no current scientific research suggesting that raw potato cuttings can effectively treat migraines when applied topically.
- bladder infections
- kidney disease
- respiratory problems
- joint pain
- arthritis
- muscle strains
Its ability to narrow blood vessels may aid in treating migraines, but no clinical trials support the use of horseradish for migraines.
Native to Asia, the Japanese honeysuckle started taking root in North America in the 1800s. It’s been used in traditional Chinese medicine to treat:
- wounds
- fever
- colds and viruses
- inflammation
- sores
- infections
Along with honeysuckle’s anticancer and antimicrobial powers, research has also identified anti-inflammatory properties in the plant’s leaves, stems, and flowers that can provide pain relief similar to that of aspirin. It may also be effective against migraine pain.
Since ancient times, people in Europe and Asia have been using mullein for medicinal purposes, treating inflammatory conditions, spasms, diarrhea, and migraines. The leaves and flowers can be used for extracts, capsules, poultices, and dried preparations. Tinctures of the plant are used in modern homeopathic therapies for migraine treatment. Research has shown that mullein has diuretic properties.
Believed to be named after Achilles, the Greek mythical hero, yarrow has historically been used to heal wounds and slow blood loss. Other folk remedies encourage the use of yarrow to treat inflammatory conditions, muscle spasms, and anxiety or insomnia. More recent folk remedies have used yarrow to relieve colds, cases of flu, coughs, and diarrhea.
Yarrow has also been shown to have pain-relieving, anti-anxiety, and antimicrobial properties. Although more research is needed, the plant contains anti-inflammatory properties that may provide relief to people who experience migraines. Yarrow can be used in a variety of forms, including capsules and tinctures.
Teaberry, popularly known as wintergreen, is native to eastern North America. This edible plant, made famous by Teaberry gum, has long held a place in folk medicine for its anti-inflammatory properties. It can be used to make teas, tinctures, and oil extracts.
Teaberry also has been used historically as an astringent and as a stimulant to fight fatigue. Most important for people who experience migraines is Teaberry’s potential to treat neuralgias and headaches as well as stomach pain and vomiting.
You can brew teaberry in hot water for 3 to 4 minutes and drink the mixture to experience its healing effects.
Hops are native to Europe and western Asia and can now be found throughout North America. Once used as a food in ancient Roman culture, this flavorful plant also has significant medicinal properties. Hops have historically been used to treat:
- sleep problems
- inflammation
- infections
- Neuralgia (pain from nerve damage)
- fever
- cramps
- spasms
- anxiety
Modern medicine acknowledges the sedative effect of hops but hasn’t thoroughly studied it for its impact on migraine pain.
This perennial herb can be found throughout Europe and Asia. It’s been used as a medicinal plant since classical times. The plant has traditionally been used to relieve headaches facial swelling and pain. The leaves can be used as juice, poultice, or ointment.
The mildly sedative properties of the plant are used to treat headache and migraine pain, menstrual cramps, stress, and tension. It may help alleviate sinus headaches and congestion when used in combination with lime flowers and comfrey.
However, there have been no human clinical trials performed to demonstrate the plant’s effectiveness against migraine pain. It’s not always easy to find betony in health food stores, so you may have to grow your own or buy it online.
Betony can have a tonic effect on the body. It’s important to avoid the herb if you’re pregnant.
This deciduous tree is native to China and has been used in Chinese medicine since the first century A.D. Evodia has traditionally been used to treat abdominal pain, headaches, diarrhea, and vomiting. The fruits of the tree may also reduce blood pressure. The anti-inflammatory and pain-reducing properties of the fruit may help ease migraine pain.
Although many herbal remedies can be safe when used correctly, they may also have side effects like any prescription medication would. Some herbs can interact with medications, such as oral contraceptives or heart drugs. Herbs can be dangerous or even deadly when misused. Some have little research to back claims, verify toxicity levels, or identify potential side effects.
In addition to herbal treatments, significant research shows that diet can play a major role in migraine frequency, duration, and intensity. Potential preventive measures and treatments for migraines include:
- eating a low-fat diet
- eliminating or limiting foods that show IgG antibody production
- improving gut flora content
- eating consistently to minimize low blood sugar
Just like medications, herbs can have significant side effects on the body. Some can interact with other medicines and be dangerous or even deadly when misused. Discuss all treatment options with your doctor before use.
Consider tracking your triggers, symptoms, pain intensity and duration, and other related factors in a migraine journal or migraine app. Whether you choose pharmaceutical treatments, natural remedies, or a combination, having a thorough record of your experiences will help you and your doctor narrow down the best treatment options.
It might also be helpful to talk to others about their own experiences with migraines. Our free app, Migraine Healthline, connects you with real people who experience migraines. Ask treatment-related questions and seek advice from others who get it.
More information related to Migraine
Thank you for reading and I hope the information above will help you overcome migraine
headaches.
Thank you for reading,
Michael
Comments are welcome



Thank you for the insightful and detailed education about migraine, the possible causes and the remedies. I can already tell what might be the cause of my colleague’s frequent headache on the left side of her head. Her excessive intake of processed food accompanied by irregular eating pattern as you describe here might be the culprit. I am going to share this article with her. This is an eye-opener.
Hi Debbie,
Thank you for your comments. It is amazing how diet can cause many health problems, including migraines. I hope your friend finds this post helpful. I appreciate you sharing it with her.
All the best to you and your friend,
Michael
Hello,
Thank you for sharing such a valuable and needed article, especially in a modern world that has been led to bypass the magic healing system right around them, without being aware.
This is more important to recognise and learn as the economy and world as we once knew it is on the verge of death. Scary to some, uplifting and inspiring to the likes of your center of information, and so much more!
My story, to put it very briefly, I have suffered forever from seeing floaters, flashing lights and awful scares from early childhood, even in the dark. I have worn glasses from 12 years old yet the problem creeped up again in my 20’s.
Naturally I consulted my optician, who had no interest in any of my sleeping, eating or life patterns or routine. I went away none the wiser until a friend of a friend recommended alternative healing ways.
I can 100% say that the only way we can life to our fullest, and healthiest is to adapt a natural lifestyle, using herbs, plants and the like for our benefitial heath
Hi, freefromtheboss,
Thank you for your comments. I am sorry to hear about the health problems you are going through. I did write a post on insomnia along with herbal treatments. I hope you will find something that may help you there:
https://empoweryourlifestyles….
Wishing you all the best,
Michael
Hello there! Thank you for sharing this very important piece of information with us, I find it very useful, informative and commendable. your thoughts are really valuable. I am a panel beater so having migraine is something that happens frequently and its making me terrible at my job. Thank you for giving ways to relieve migraine, now I can do a greater service to my clients. thanks a lot
Hi Philebur,
Thank you for your comments. I hope your migraines go away and you find some relief.
Best wishes,
Michael
Heat, lack of proper sleep, foods that contains vegetable oil made from maize, these are the major things I have noticed that cause migraine headaches in my head.
Whenever I am in a place that is not properly ventilated and the atmosphere is hot I am sure to get a bout of migraine attacks.
Some people, lots of people do not know these things or do not even notice the things that causes them to have migraine headaches. This article is so detailed and accurate about this topic. Thanks for a very good analysis of the situation.
Hi, Samikingss,
Thank you for your comments. I also appreciate you adding more reasons that cause migraines. Diet and sleep are very important. Please if you continue to get regular migraines to check with your doctor. There could be other reasons, blood pressure should be checked.
All the best,
Michael