What is melanoma skin cancer?
Blue indicates link
Melanoma skin cancer starts in melanocyte cells of the skin. A cancerous (malignant) tumor is a group of cancer cells that can grow into and destroy nearby tissue. It can also spread (metastasize) to other parts of the body.

Melanocytes make melanin. Melanin gives skin, hair, and eyes their color. The skin is the body’s largest organ and covers your entire body. It protects you against harm from things around you like the sun, hot temperatures, and germs. The skin controls body temperature, removes waste products from the body through sweat, and gives a sense of touch. It also helps make vitamin D.
Melanocytes can group together and form moles on the skin. They appear as bumps or spots that are usually brown or pink. Most people have a few moles. Moles are non-cancerous (benign) tumors.
But in some cases, changes to melanocytes can cause melanoma skin cancer. A change in the color, size, or shape of a mole is usually the first sign of melanoma skin cancer. There are 4 main types of melanoma skin cancer. Superficial spreading melanoma is the most common type. The other types are nodular melanoma, lentigo malignant melanoma, and acral lentiginous melanoma.
Melanoma skin cancer can also start in other parts of the body where melanocytes are found, but these types of melanoma are rare. Mucosal lentiginous melanoma develops on the thin, moist lining of some organs or other parts of the body, such as the nasal passages, mouth, and anal canal. Intraocular melanoma starts in the eye.
Another type of skin cancer is non-melanoma, and it’s more common than melanoma. Non-melanoma skin cancers start in basal cells and squamous cells of the skin.
What is non-melanoma skin cancer?
Non-melanoma skin cancer starts in the cells of the skin. A cancerous (malignant) growth is a group of cancer cells that can grow into and destroy nearby tissue. It can also spread (metastasize) to other parts of the body, but this is rare with non-melanoma skin cancer.
The skin is the body’s largest organ. It covers your entire body and protects you against harmful factors from the environment such as the sun, hot temperatures, and germs. The skin controls body temperature, removes waste products from the body through sweat, and provides a sense of touch. It also helps make vitamin D.
Cells in the skin sometimes change and no longer grow or behave normally. These changes may lead to non-cancerous (benign) growths such as dermatofibromas, moles, skin tags, and warts.
Changes to cells of the skin can also cause precancerous conditions. This means that the abnormal cells are not yet cancer, but there is a chance that they may become cancer if they aren’t treated. A precancerous condition of the skin is actinic keratosis.
But in some cases, changes to skin cells can cause non-melanoma skin cancer. Most often, non-melanoma skin cancer starts in round cells called basal cells found in the top layer of the skin (epidermis). This type of cancer is called basal cell carcinoma (BCC) and makes up about 75%–80% of all skin cancers. Non-melanoma skin cancer can also start in squamous cells of the skin, which are flat cells found in the outer part of the epidermis. This type of cancer is called squamous cell carcinoma (SCC) and makes up about 20% of all skin cancers. BCC and SCC tend to grow slowly and are often found early.
Rare types of non-melanoma skin cancer can also develop. These include Merkel cell carcinoma and cutaneous T-cell lymphoma.
Finding skin cancer early:
When skin cancer (non-melanoma or melanoma) is found and treated early, the chances of successful treatment are better. Get regular health checkups and see your doctor if you have any symptoms or are worried about your health.
If you have a higher-than-average risk, you may need to visit your doctor more often to check for skin cancer. Talk to your doctor about what can help find skin cancer early including checking your skin and having skin exams by a trained health professional.
Checking your skin:
You should check your skin regularly for changes. This will help you get to know what is normal for your skin and notice when something may be wrong. See your doctor if you find any changes in your skin.
How to check your skin:
Check your skin in a well-lit room. Use a mirror so you can look closely at your entire body.
Raise your arms and look at the right and left sides of your body in the mirror. Check your underarm areas and both sides of your arms. Look at your hands, each finger, between your fingers and your fingernails.
Look at the back, front, and sides of your legs. Look at the tops and soles of your feet, your toenails, and the spaces between your toes. Also, check your genital area and between your buttocks.
Look at your face, neck, back of your neck, and your scalp. Use a hand mirror and full-length mirror, along with a comb, to check your scalp.
Have someone you trust help you check areas that are hard to see.
What to look for:
Skin cancer usually starts as an abnormal area or change on any part of the skin. Look for and make note of any changes including:
- a sore that doesn’t heal or comes back after healing
- a mole or sore that oozes, bleeds, or is crusty
- a change in the color, size, or shape of a mole or birthmark
- a growth or area that is itchy, irritated, or sore
- rough or scaly red patches
- small, smooth, and shiny lumps that are pearly white, pink, or red
- pale white or yellow flat areas that look like scars
- raised lumps that indent in the center
What to do if you find a change on your skin:
Tell your doctor as soon as possible if you notice any changes to your skin. Your doctor will do a skin exam to check the specific area and look for any signs of skin cancer. You may be referred to a specialist, such as a dermatologist or plastic surgeon. Your doctor may do a skin biopsy to check for cancer.
Skin exams:
A skin exam allows your doctor or another trained health professional to look for any signs of skin cancer or abnormal areas of your skin. It is often done as part of a yearly health checkup. Getting regular and thorough skin exams can help find skin cancer early.
Signs and symptoms of non-melanoma skin cancer:
Non-melanoma skin cancer usually starts as an abnormal area or change on any part of the skin. How non-melanoma skin cancer looks often depends on the type of cancer. Other health conditions can also look like non-melanoma skin cancer. See your doctor if you have any changes to your skin.
The following are common signs and symptoms of basal cell carcinoma (BCC) and squamous cell carcinoma (SCC), the most common types of non-melanoma skin cancer.
Basal cell carcinoma usually develops in areas of skin exposed to the sun, especially the head, face, and neck. It can also develop in the central part of the body (trunk). BCC may appear on the skin as:
- a sore that doesn’t heal or comes back after healing
- pale white or yellow flat areas that look like scars
- raised and scaly red patches
- small, smooth, and shiny lumps that are pearly white, pink, or red
- a pink growth with raised edges and indents in the center
- a growth that has small blood vessels on the surface
- a sore that bleeds
- a growth or area that is itchy
Squamous cell carcinoma usually develops on areas of skin exposed to the sun, but it can also be found on the skin around the genitals and anus. It can occur on the skin of scars, sores, ulcers, and burns. SCC may appear on the skin as:
- a sore that doesn’t heal or comes back after healing
- rough or scaly red patches with irregular borders
- raised lumps that indent in the center
- a growth that looks like a wart
- a sore that is crusty or bleeds easily
- a growth or area that is itchy, irritated, or sore
Diagnosis of non-melanoma skin cancer:
Diagnosing non-melanoma skin cancer usually begins with a visit to your family doctor. Your doctor will ask you about any signs or symptoms you have and will do a skin exam. Based on this information, your doctor may refer you to a specialist, such as a dermatologist or a surgeon.
The process of diagnosis may seem long and frustrating. It’s normal to worry, but try to remember that other health conditions can cause similar signs and symptoms as non-melanoma skin cancer. It’s important for the healthcare team to rule out other reasons for a health problem before making a diagnosis of non-melanoma skin cancer.
A health history, skin exam, and skin biopsy are commonly used to rule out or diagnose non-melanoma skin cancer.
Health history and skin exam:
Your health history is a record of your symptoms, risk factors, and all the medical events and problems you have had in the past. In taking a health history, your doctor will ask questions about your history of:
- Sun exposure and indoor tanning
- signs or symptoms that suggest non-melanoma skin cancer
- actinic keratosis, which is a precancerous condition of the skin
- inherited conditions, such as xeroderma pigmentosum and basal cell nevus syndrome
Your doctor may also ask about a family history of skin cancer, both non-melanoma and melanoma.
A skin exam allows your doctor to look for any signs of skin cancer or an abnormal area of skin. During a skin exam, your doctor will check the entire surface of your skin, especially areas of skin exposed to the sun.
Skin biopsy:
During a skin biopsy, the doctor removes tissue or cells from the skin for testing in a lab. The report from the pathologist (a doctor who specializes in the causes and nature of disease) will confirm whether or not cancer cells are present in the sample. The type of biopsy used often depends on the growth or abnormal area looks like and where it is located.
Shave biopsy shaves off growth or abnormal area of skin using a flexible razor blade or a surgical knife (scalpel). It is usually used for raised growth. It can also be used for flat abnormal areas that are only on the outer surface of the skin (superficial).
Punch biopsy removes a round area of skin using a sharp tool called a punch or trephine. It is usually used when the growth or abnormal area is under the skin or seems to have grown deep into the skin.
Excisional biopsy (a type of surgical biopsy) removes the entire growth or abnormal area using a scalpel. It is usually done when the doctor thinks the whole growth or area needs to be examined to make a proper diagnosis.
Determining the extent of the melanoma:
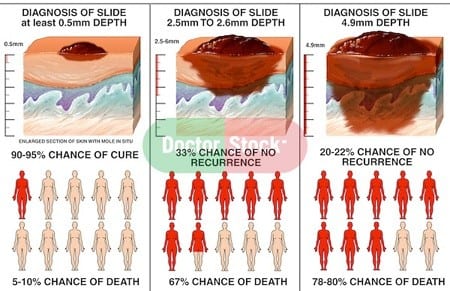
If you receive a diagnosis of melanoma, the next step is to determine the extent (stage) of cancer. To assign a stage to your melanoma, your doctor will:
- Determine the thickness. The thickness of a melanoma is determined by carefully examining the melanoma under a microscope and measuring it with a special tool. The thickness of melanoma helps doctors decide on a treatment plan. In general, the thicker the tumor, the more serious the disease. Thinner melanomas may only require surgery to remove the cancer and some normal tissue around it. If the melanoma is thicker, your doctor may recommend additional tests to see if the cancer has spread before determining your treatment options.
- See if the melanoma has spread to the lymph nodes. If there’s a risk that the cancer has spread to the lymph nodes, your doctor may recommend a procedure known as a sentinel node biopsy. During a sentinel node biopsy, a dye is injected in the area where your melanoma was removed. The dye flows to the nearby lymph nodes. The first lymph nodes to take up the dye are removed and tested for cancer cells. If these first lymph nodes (sentinel lymph nodes) are cancer-free, there’s a good chance that the melanoma has not spread beyond the area where it was first discovered.
- Look for signs of cancer beyond the skin. For people with more advanced melanomas, doctors may recommend imaging tests to look for signs that the cancer has spread to other areas of the body. Imaging tests may include X-rays, CT scans, and positron emission tomography (PET) scans. These imaging tests generally aren’t recommended for smaller melanomas with a lower risk of spreading beyond the skin.
Other factors may go into determining the risk that the cancer may spread (metastasize), including whether the skin over the area has formed an open sore (ulceration) and how many dividing cancer cells (mitoses) are found when looking under a microscope.
Melanoma is staged using the Roman numerals 0 through IV. At stage 0 and stage I, melanoma is small and has a very successful treatment rate. But the higher the numeral, the lower the chances of a full recovery. By stage IV, the cancer has spread beyond your skin to other organs, such as your lungs or liver.
Treatments for melanoma skin cancer:
If you have melanoma skin cancer, your healthcare team will create a treatment plan just for you. It will be based on your health and specific information about cancer. When deciding which treatments to offer for melanoma skin cancer, your healthcare team will consider:
- the stage of cancer – whether it is early stage, locoregional or metastatic
- the risk that cancer will come back (recur)
- where the cancer is located
- How treatments will affect how you look
- your personal preferences (what you want)
You may be offered one or more of the following treatments for melanoma skin cancer.
Surgery:
Surgery is the main treatment for most melanoma skin cancers. Depending on the stage and risk of cancer coming back, you may have one or more of the following types of surgery.
Wide local excision removes cancer along with some normal tissue around it (called the surgical margin). It is the first treatment for early-stage, locoregional, and locally recurrent melanoma skin cancers.
Sentinel lymph node biopsy (SLNB) finds and removes the first lymph node (or first few lymph nodes) in a group of lymph nodes to see if it contains cancer cells. It may be done for early-stage melanoma skin cancers when the tumor is thick.
Complete lymph node dissection removes a group of lymph nodes from the body. It is done for locoregional or locally recurrent melanoma skin cancer that has spread to nearby lymph nodes.
Reconstructive surgery repairs the skin and nearby areas after the tumor is removed. When a large area of skin has been removed to make sure the cancer is completely gone, the doctor rebuilds the area using a piece of skin from another part of the body, called a skin graft or skin flap.
Surgery for metastases may be done to remove metastatic melanoma skin cancer that has spread to only one area or a few areas on or just under the skin, or in the lung, liver, brain, or small intestine.
Immunotherapy:
Immunotherapy uses drugs to help the body’s immune system to fight cancer cells. It is sometimes used after surgery to lower the risk of cancer coming back, or shrink and control the growth of melanoma skin cancer when surgery can’t be done.
Radiation therapy:
External beam radiation therapy uses a machine to direct a beam of radiation to the area of the skin and a small amount of nearby tissue. It is sometimes used after surgery to lower the risk of cancer coming back, or as palliative therapy to control symptoms from advanced melanoma skin cancer.
Chemotherapy:
Chemotherapy uses anticancer (cytotoxic) drugs to destroy cancer cells. It can be given throughout the body (called systemic chemotherapy) for metastatic melanoma skin cancer. It may be given directly into an arm or leg (called regional chemotherapy) for locally recurrent melanoma skin cancer that is only in one limb.
Targeted therapy:
Targeted therapy uses drugs to target specific molecules (such as proteins) on or inside cancer cells to stop the growth and spread of cancer and limit harm to normal cells. It is usually used in people with metastatic melanoma skin cancer who have certain gene changes (mutations) in the BRAF gene.
If you can’t have or don’t want cancer treatment:
You may want to consider a type of care to make you feel better without treating cancer itself. This may be because the cancer treatments don’t work anymore, they’re not likely to improve your condition or they may cause side effects that are hard to cope with. There may also be other reasons why you can’t have or don’t want cancer treatment.
Follow-up care:
Follow-up after treatment is an important part of cancer care. You will need to have regular follow-up visits, especially in the first 5 years after treatment has finished. These visits allow your healthcare team to follow your progress and recovery from treatment.
Coping and support:
A cancer diagnosis can change your life forever. Each person finds his or her own way of coping with the emotional and physical changes cancer brings. But when you’re first diagnosed with cancer, sometimes it’s difficult to know what to do next.
Here are some ideas to help you cope:
-
-
-
- Learn enough about melanoma to make decisions about your care. Ask your doctor about your cancer, including your treatment options and, if you like, your prognosis. As you learn more about cancer, you may become more confident in making treatment decisions.
- Keep friends and family close. Keeping your close relationships strong will help you deal with your cancer. Friends and family can provide the practical support you’ll need, such as helping take care of your home if you’re in the hospital. And they can serve as emotional support when you feel overwhelmed by cancer.
- Find someone to talk with. Find a good listener who is willing to listen to you talk about your hopes and fears. This may be a friend or family member. The concern and understanding of a counselor, medical social worker, clergy member, or cancer support group also may be helpful.
- Ask your doctor about support groups in your area. Other sources of information include the National Cancer Institute and the American Cancer Society.
- ALWAYS TALK WITH YOUR DOCTOR.
HERBAL Alternative Remedies In Treating Melanoma/Skin Cancer:
-
- Astragalus
- This herb is the most effective natural remedy for melanoma. The extracts of astragalus have antioxidant, anti-tumor, and anti-inflammatory properties that enhance the immune system of the skin and help in the buildup of anticancer skin cells. The herb is so effective that doctors suggest its use even when the condition of a patient is critical and he/she is undergoing chemotherapy.
- Turmeric Extract
- We already know that turmeric is a very good antiseptic agent and can be used to cure and prevent skin ailments. An extract of turmeric known as curcumin has shown anti-melanoma properties in medical tests. This extract must be taken with food or mixed with other medicines for daily consumption.
- Mushroom Cordyceps is a variety of mushroom that has been clinically tested to show results against the growth of skin cells that are affected by melanoma. Clean and cook cordyceps mushrooms properly before consumption to avoid allergies or rashes. The element cordycepin in cordyceps prevents the spread of melanoma.
- Green Tea The EGCG extract in green tea is an effective herbal treatment for melanoma. If melanoma is detected in your skin, drink at least three glasses of green tea every day. You can also apply green tea extracts on the affected skin.
- Tea Tree Oil The terpene in tea tree oil is a form of melaleuca alternifolia. According to medicine, the latter is a component that stops the in-vitro growth of skin cells affected by skin cancer. Rosemary Extracts of this exotic herb contains carnosol that has been medically tested to show anti-carcinogenic and antioxidant qualities. Rosemary also has small quantities of resveratrol (also found in grapes) which prevents the growth of cancer-affected skin cells and thus cures melanoma naturally. Raspberry Extract Pluck red raspberries for the purpose of killing melanoma-affected skin cells. Components allantoin and ascorbyl palmitate present in raspberry work to inhibit the spread of melanoma to neighboring areas, thus curing the disease.
- Skin Hydrators It is very important to keep skin hydrated because when the skin is dry or wrinkled, skin cancer spreads faster. Drink lots of water and vegetable juice to cure melanoma naturally.
- Personal Note:
-
It is summer, and we all like to enjoy being able to enjoy the sunshine. Please use proper sunscreen to protect your skin from ultraviolet rays.
Enjoy your summer, but remember too much time in the sun can be harmful. Especially if you are not using a protective sunscreen.
Thank you for reading,
Michael
Comments are welcome.
This is high-quality information on this topic. I think it is accurate to share this kind of information now that summer is coming. As you mention, you can enjoy the sun this summer, but taking care of yourself. It is great to have access to natural alternatives in the treatment of this harmful disease-
Hi Nicole,
Thank you for your comments. You are so right. With summer approaching we need to protect ourselves from the sun’s powerful UV rays.
All the best,
Michael
Hello there, thanks a lot for sharing this beautiful content here with us. I must say i really did enjoyed going through your article as it contains valuable information’s one needs to be aware of. I think it is very necessary to understand and be aware of these signs and symptoms so one can find treatment early, thanks for sharing this.
Hi Philebur,
Thank you for your comments.
Michael
I took my my time to read this article and I found it very helpful as it concern our health and life’s, this is a great content as a novice in health matters can easily understand what you are talking about. The importance of caring for our skin cannot be over emphasis. Thank you once more for sharing
Hi petergeorge,
Thank you for your comments. We are in control of our bodies, and we owe it to ourselves to take the necessary steps to protect it. Too much-unprotected sunshine can harm us.
Best wishes,
Michael
Hello there a big thanks to you for sharing this insightful and educatinonal article on the topic titled: treatments for Melanoma skin cancer. Melanoma skin cancer is one dangerous cancer, I do not find it funny at all. Anyways this article is indeed filled with lots of information on the melanoma skin cancer and how it could be managed. Thanks, I believe this will help someone out there.
Hi Sheddy,
Thank you for your comments. Every time we are in the bright sunshine, as great as it may feel we need to protect ourselves with adequate sunscreen.
Best wishes,
Michael