There are Five Types of Viral Hepatitis.
Blue indicates link
Hepatitis A, B, C, D, and E
What is Hepatitis?
Hepatitis refers to an inflammatory condition of the liver. It’s commonly caused by a viral infection, but there are other possible causes of hepatitis. These include autoimmune hepatitis and hepatitis that occurs as a secondary result of medications, drugs, toxins, and alcohol. Autoimmune hepatitis is a disease that occurs when your body makes antibodies against your liver tissue.
Your liver is located in the right upper area of your abdomen. It performs many critical functions that affect metabolism throughout your body, including:
- bile production, which is essential for digestion
- filtering of toxins from your body
- excretion of bilirubin (a product of broken-down red blood cells), cholesterol, hormones, and drugs
- breakdown of carbohydrates, fats, and proteins
- activation of enzymes, which are specialized proteins essential to body functions
- storage of glycogen (a form of sugar), minerals, and vitamins (A, D, E, and K)
- synthesis of blood proteins, such as albumin
- Synthesis of clotting factors
According to the Centers for Disease Control and Prevention (CDC), approximately 4.4 million Americans are currently living with chronic hepatitis B and C. Many more people don’t even know that they have hepatitis.
Treatment options vary depending on which type of hepatitis you have. You can prevent some forms of hepatitis through immunizations and lifestyle precautions.
Hepatitis C:
Hepatitis C comes from the hepatitis C virus (HCV). Hepatitis C is transmitted through direct contact with infected body fluids, typically through injection drug use and sexual contact. HCV is among the most common bloodborne viral infections in the United States. Approximately 2.7 to 3.9 million Americans are currently living with a chronic form of this infection.
Hepatitis C is an infectious disease caused by the hepatitis C virus (HCV) that primarily affects the liver. During the initial infection, people often have mild or no symptoms. Occasionally a fever, dark urine, abdominal pain, and yellow-tinged skin occurs. The virus persists in the liver in about 75% to 85% of those initially infected. Early on chronic infection typically has no symptoms. Over many years, however, it often leads to liver disease and occasionally cirrhosis. In some cases, those with cirrhosis will develop serious complications such as liver failure, liver cancer, or dilated blood vessels in the esophagus and stomach.
HCV is spread primarily by blood-to-blood contact associated with intravenous drug use, poorly sterilized medical equipment, needlestick injuries in healthcare, and transfusions. Using blood screening, the risk from a transfusion is less than one per two million. It may also be spread from an infected mother to her baby during birth. It is not spread by superficial contact. It is one of five known hepatitis viruses: A, B, C, D, and E. Diagnosis is by blood testing to look for either antibodies to the virus or its RNA. Testing is recommended for all people who are at risk.
There is no vaccine against hepatitis C. Prevention includes harm reduction efforts among people who use intravenous drugs and testing donated blood. Chronic infection can be cured about 95% of the time with antiviral medications such as sofosbuvir or simeprevir. Peginterferon and ribavirin were earlier-generation treatments that had a cure rate of less than 50% and greater side effects. Getting access to the newer treatments, however, can be expensive. Those who develop cirrhosis or liver cancer may require a liver transplant. Hepatitis C is the leading reason for liver transplantation, though the virus usually recurs after transplantation.
An estimated 143 million people (2%) worldwide are infected with hepatitis C as of 2015. In 2013, about eleven million new cases occurred. It occurs most commonly in Africa and Central and East Asia. About 167,000 deaths due to liver cancer and 326,000 deaths due to cirrhosis occurred in 2015 due to hepatitis C. The existence of hepatitis C – originally identifiable only as a type of non-A non-B hepatitis – was suggested in the 1970s and proven in 1989. Hepatitis C infects only humans and chimpanzees.
Hepatitis C is a sneaky virus. You may not have any symptoms at all. Most people don’t. Your doctor could check your liver and see only a little damage. You might not get diagnosed until he spots a problem with your liver enzymes after a routine blood test.
More than 3 million Americans have a long-term infection from the hepatitis C virus (HCV). Anyone who has this disease can give it to someone else through blood and other bodily fluids.
Once you’ve learned what situations make you likely to catch it, though, you can take steps to protect yourself or get diagnosed and treated.
Early Signs and Symptoms of Acute Hepatitis C:
The disease is called acute hepatitis C when you first get it. The symptoms are similar to those of the flu, but you might not have symptoms at all.
They may include:
- Belly pain
- Clay-colored poop
- Dark urine
- Fatigue
- Fever
- Jaundice (yellow tint to your skin or eyes)
- Joint pain
- Poor appetite
- Nausea
- Vomiting
Symptoms usually show up between 2 and 12 weeks after exposure to the virus.
Chronic Hepatitis C Symptoms:
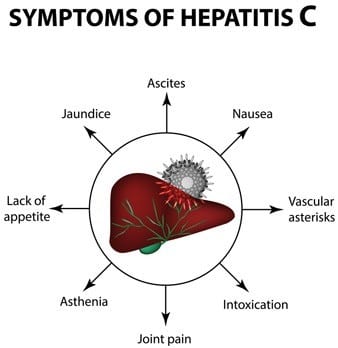
If you don’t get diagnosed and treated, you could have the disease for years and not know it. Doctors call this the chronic form because it lasts a long time. Some people who’ve had it for a while get liver cancer or scarring of the liver, which is called cirrhosis.
In addition to the above symptoms, signs that your liver isn’t working the way it should include:
- Ascites — fluid buildup in your belly
- Easy bleeding
- Easy bruising
- Hepatic encephalopathy — confusion, drowsiness, and slurred speech
- Hives or rashes
- Itchy skin
- Spider angiomas — spidery blood vessels under your skin
- Swollen legs
- Weight loss
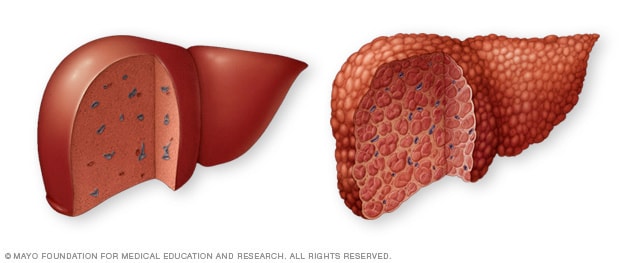
Symptoms of Cirrhosis From Untreated Hepatitis C:
You could get scarring of the liver, called cirrhosis after you’ve had hepatitis C for 20 or 30 years. If you have it, you might:
- Retain water
- Bleed and bruise easily
- Notice skin and eyes turning yellow with jaundice
Complications:
Normal liver vs. liver cirrhosisOpen pop-up dialog box
Hepatitis C infection that continues over many years can cause significant complications, such as:
- Scarring of the liver (cirrhosis). After decades of hepatitis C infection, cirrhosis may occur. Scarring in your liver makes it difficult for your liver to function.
- Liver cancer. A small number of people with hepatitis C infection may develop liver cancer.
- Liver failure. Advanced cirrhosis may cause your liver to stop functioning.
Does Hep C Always Become Chronic?
No. Doctors aren’t sure how it works but between 15% and 25% of adults who have it clear the virus from their bodies without treatment. You might hear this called spontaneous clearance.
Who’s at Risk for Hepatitis C?
The odds are higher that you’ll get hepatitis C if you:
- Had a blood transfusion before 1992. A screening test for HCV went into use that year. Before then, this was the main cause of most new cases in the U.S. With routine blood screening for HCV and improvements in the test in mid-1992, transfusion-related hepatitis C has virtually disappeared.
- Use needles to take illegal drugs. This is one of the most common ways to get hep C. Up to 80% of new users get the disease within 6 to 12 months.
- Snort cocaine. People who share straws or other tools to inhale this drug raise their risk.
- Workaround blood or needles. Doctors, nurses, and people in the lab get hepatitis C more often than others. They’re more likely to come in contact with blood and get accidental needle sticks.
- Are on dialysis. You can get the disease from equipment that isn’t properly cleaned or should have been thrown away but was reused.
- Have a risky sex life. If you have more than one partner or sleep with people who have sexually transmitted diseases, particularly HIV, you’re more likely to get hep C than people who don’t.
- Have a spouse or partner who has it, or care for someone who does. Being in close daily contact with an infected person puts you at risk.
- Have body piercings or tattoos. Equipment and supplies can be infected with HCV, but this type of infection doesn’t happen often. To be on the safe side, make sure all tools are sterile or disposable, even the tattoo ink.
- Were born to a mother with hepatitis C. Moms can pass the disease to babies, but it doesn’t happen all the time. If the mother has HIV and hepatitis C, there’s more of a chance the baby will get infected.
- Hepatitis spreads easily when people share things that pierce the skin, like:
-
- Needles or other methods to inject drugs
- Tattoo equipment
- Piercing equipment
Hepatitis C Transmission:
If you’ve just been diagnosed with hepatitis C, you may wonder how you got it and worry about passing on the virus to a loved one. If you’ve had the disease for a long time without knowing it, you could dwell on every little incident in the past where you might have accidentally exposed a family member to the disease.
It’s important to remember that hepatitis C isn’t easy to catch. If you take a few precautions, it’s almost impossible to pass on the disease to someone else.
How Does Hepatitis C Spread?
Hepatitis C is spread only through exposure to an infected person’s blood.
High-risk activities include:
- Sharing drug use equipment. Anything involved with injecting street drugs, from syringes to needles, to tourniquets, can have small amounts of blood on it that can transmit hepatitis C. Pipes and straws to smoke or snort drugs can have blood on them from cracked lips or nosebleeds. Get into a treatment program if you can. At the very least, don’t share needles or equipment with anyone else.
- Sharing tattoo or piercing tools. Nonsterile items and ink can spread contaminated blood.
- Blood transfusions in countries that don’t screen blood for hepatitis C.
- Nonsterile medical equipment. Tools that aren’t cleaned properly between use can spread the virus.
- Blood or cutting rituals. Sharing the tools or exchanging blood can transmit hepatitis C.
Medium-risk activities include:
- Sharing or not disposing of grooming and hygiene supplies. This includes razors, toothbrushes, nail clippers, or anything else that could have your blood on it. Cover any open wounds or sores with bandages. Carefully dispose of tampons, sanitary napkins, tissues, used bandages, and anything else that might have your blood on it.
- Unprotected sex. It’s rare, but you can spread and catch it from sex, especially during menstruation or certain sex practices like fisting. It’s more likely you’ll spread it if you have HIV or another sexually transmitted infection.
- Pregnancy and birth. There’s a small risk for a mother to pass the disease on to her child before or during birth. The odds go up if the mother has HIV.
- Needle-stick injuries. Healthcare workers and caregivers are most likely to get it this way.
Diagnostic Tests for the Hepatitis C Virus:
You can be infected with the hepatitis C virus and have no symptoms. Your doctor could find it when he checks your blood and sees that your level of certain liver enzymes is high. If that happens, he’ll follow up with other tests to confirm you have the disease. Who Should Get Screened for Hepatitis C? Some doctors say you should get tested at least once no matter what.
Definitely, get screened if any of these things apply to you:
Were born between 1945 and 1965. Currently using or injecting drugs. Ever injected drugs — even if it was just once or a long time ago? Have abnormal alanine aminotransferase levels (ALT). Had a blood transfusion, blood components, or an organ transplant before July 1992. Got clotting factor concentrates made before 1987. Received blood from a donor who later tested positive for the hepatitis C virus. (HCV) Health care workers, first responders, and others whose work exposes them to HCV-infected needles. Children born to women with HCV.
Why Should You Get Tested?
You can have hep C with no symptoms. The test is quick and easy. You’ll protect family and friends. Treatment can suppress the virus and maybe even cure you. Early treatment prevents cirrhosis and liver failure. Hepatitis C Testing and DiagnosisDoctors will start by checking your blood for anti-HCV antibodies: These are proteins your body makes when it finds the hep C virus in your blood. They usually show up about 12 weeks after infection.
How long does it take to get results?
It usually takes a few days to a week to get results, though a rapid test is available in some places.
What do the results mean?
Non-Reactive or negative:
You don’t have hep C. If you’ve been exposed in the last 6 months, you’ll need to be retested.
Reactive or positive:
You have hep C antibodies, and you’ve been infected at some point. You’ll need another test to make sure.
Hepatitis C Treatments:
Hepatitis C is the No. 1 cause of liver cancer and liver transplants. It’s brought on by a virus you can catch if you come into contact with contaminated blood. You could get it from an unclean tattoo needle, for example. Sometimes, it spreads during sex.
It’s curable. But curing it hasn’t always been easy or comfortable. For decades, you needed painful shots of a medicine called interferon and a pill called ribavirin. These drugs didn’t target the virus that made you sick. Instead, they amped up your immune system so you’d fight it the way you do when you get the flu.
But the treatment didn’t always get the virus out of your body. Cure rates hovered around 50%. And people who stuck with the yearlong treatment – not all did – had to live with chemo-like side effects.
These days, more and more people can get rid of the virus by simply taking a pill, at home, for just a few weeks. There are several ways to do it without having to get shots.
How They Work:
There’s no one-size-fits-all option. There are many different types, or “genotypes,” of hepatitis C. Type 1 is the most common. This is important to understand when you talk to your doctor. Not all meds work on all types. Which medicine is best for you also depends on how much liver scarring (cirrhosis) you have.
Your doctor might call these new drugs direct-acting antivirals. They zoom in on the virus that’s making you sick. Each drug works in a slightly different way. But in general, the medicine interferes with proteins that help the virus grow or spread.
Most of the time, these meds remove all traces of the virus from your blood within 12 weeks. This is called sustained virologic response (SVR), and it’s what doctors look for to tell if you’re cured. How long you’ll need treatment can vary. It may range from 8 to 24 weeks.
Hepatitis C Prevention:
The hepatitis C virus can be transmitted only through blood. But exposure to tiny amounts of blood is enough to infect you.
How to Prevent the Spread of Hep C:
- Never share needles. Intravenous drug users have the highest chance of getting infected with hepatitis C because they share needles. Besides needles, the virus may be present in other equipment used with illicit drugs. Even sharing a straw or dollar bill when snorting cocaine could transmit hepatitis C. Bleeding in the nose frequently happens when taking cocaine this way, and microscopic droplets may enter the straw and be passed on to the next user, even if they can’t be seen.
- Avoid direct exposure to blood or blood products. If you are a medical worker or health care provider, avoid coming into direct contact with blood. Any tools that draw blood in the workplace should be thrown out safely or sterilized to prevent hepatitis C infection.
- Don’t share personal care items. Many items that we use on a daily basis will occasionally be exposed to blood. Often, people will cut themselves while shaving, or their gums will bleed while brushing their teeth. Even small amounts of blood can infect someone, so it is important not to share items such as toothbrushes, razors, nail and hair clippers, and scissors. If you already have hepatitis C, make sure you keep your personal items, such as razors and toothbrushes, separate and out of children’s reach.
- Choose tattoo and piercing parlors carefully. Only use a licensed tattoo and piercing artist who does the right sanitary procedures. A new, disposable needle and ink well should be used for each customer. If in doubt, ask about their disposable products and sanitary procedures before getting a tattoo or piercing.
- Practice safe sex. It is rare for hepatitis C to be transmitted through sexual intercourse, but there is a higher chance of getting hepatitis C if you have HIV, another sexually transmitted disease, multiple sex partners, or if you engage in rough sex.
Can Herbal Remedies Help?
Milk thistle:
Milk thistle is an herb thought to have properties that promote liver health. It’s sometimes sold as Silybum marianum, or as silymarin. Side effects may include nausea, diarrhea, and abdominal bloating. You may also experience headaches, skin reactions such as eczema or other allergic reactions, or insomnia. Still, it’s well tolerated by most people. Silymarin is the most widespread supplement taken for liver disease.
However, the National Center for Complementary and Alternative Medicine (NCCAM) conducted a clinical trial that found milk thistle to be no more effective than a placebo for stopping liver damage.
Zinc supplements are sometimes touted as a good therapy for hepatitis C. Zinc is essential to liver function. A deficiency of this mineral can impair cellular immunity so supplements may be a complementary treatment for hepatitis C.
However, there is no evidence to suggest that zinc can halt the progression of hepatitis C. You shouldn’t use it as a sole treatment either. Excessive amounts of zinc can be toxic.
Colloidal silver:
Colloidal silver is often cited as a treatment for hepatitis C. Some believe that it can reduce symptoms of the virus, but this is inaccurate. There are no studies that currently support this theory. In fact, the U.S. Food and Drug Administration (FDA) warns that colloidal silver is not considered a safe or effective treatment for any disease. Serious side effects include argyria, the permanent, grayish discoloration of the skin.
Colloidal silver isn’t safe to take as a treatment for hepatitis C and shouldn’t be taken even by healthy individuals.
Probiotics:
Probiotics are live microscopic organisms (bacteria) much like those you already have in your body. These good bacteria may benefit your overall health. Most people can tolerate supplementing with probiotics without harmful side effects. Research into the benefits of probiotics is ongoing. To date, there is no solid evidence that probiotics can halt the progression of hepatitis C or lessen its symptoms.
Other supplements:
Other supplements that have been studied include glycyrrhizin (from licorice root), lactoferrin (a protein found in milk), SAMe (a chemical naturally found in your body), TJ-108 (herbs used in Japanese Kampo medicine), Schisandra (the berries of the plant), oxymatrine (the extract of sophora root), and thymus extract(from the glands of cows). According to the NCCAM, there is no proof that any dietary supplement is an effective treatment for hepatitis C.
Acupuncture:
Acupuncture is a form of traditional Chinese medicine. It’s where thin needles are inserted through your skin at specific points to stimulate your healing and well-being. It’s generally used to treat pain and nausea. There are no published studies regarding the use of acupuncture to treat hepatitis C. It’s also important to know that you can transmit hepatitis C to another person through the use of needles.
Yoga:
There are no studies that show yoga is an effective treatment for hepatitis C. However, yoga movements can help you learn to control breathing and improve concentration. Many people who practice yoga report an improved sense of general well-being. There is no evidence to suggest that yoga has any adverse effects on people with hepatitis C.
Qigong:
Qigong is a traditional Chinese practice combining controlled breathing techniques and easy movements. It’s thought to promote harmony and strength. There are no studies to confirm that this energy-conserving practice can help treat hepatitis C. But it may promote a more positive feeling. There is also no indication that qigong can harm your health.
Lifestyle:
Alcohol can speed up the progression of hepatitis C, so consider eliminating it from your diet.
Additionally, many medications can cause liver damage. Read the labels carefully. Discuss the potential side effects of all your medications and supplements with your doctor. Some herbs are harmful to the liver, which is already compromised if you have hepatitis C.
To prevent spreading hepatitis C to others, don’t let anyone come into contact with your blood. Bandage all wounds, even small ones. Don’t share personal care items like toothbrushes and razors. Don’t donate or list yourself as a blood or organ donor. Always inform your healthcare providers, including dentists, that you have hepatitis C.
Key points to consider:
No vitamin or herbal supplements are proven effective in treating hepatitis C, according to the Centers for Disease Control and Prevention (CDC). Talk to your doctor before taking dietary supplements or herbal remedies. Even natural products can be harmful. It’s important to understand how they may interact with each other or with medications. If you’re considering going off your medication, talk to your doctor first. A healthy diet and moderate exercise may help your overall health.
Please Always Consult With Your Doctor If You Feel You Are At Risk or Show Any Symptoms
Thank you for reading,
Michael
Comments are welcome.
I think this topic is extremely important. There are millions of people walking around completely oblivious to the fact that they have hepatitis. I get a frequent checkup from my doctor every so often to ensure I am healthy and in good working order. One of my worse fears is waking up and being told I have a hepatitis or other similar disease. Thanks for this article, I learnt a lot!
Hi Brandon,
Thank you for your comments. It is always better to be safe than sorry. Frequent checkups with your doctor I think is a great idea.
Best wishes,
Michael