What is Colitis?
Blue indicates link
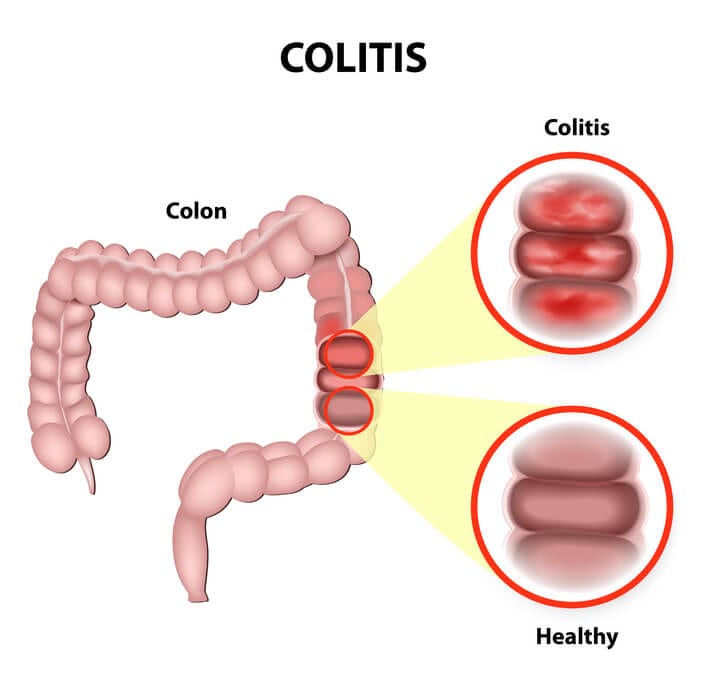
Inflammation of the inner lining of the colon. Very common (More than 500,000 cases per year in Canada) and often requires lab tests or imaging. Treatment from a medical professional is advised. It can last several months or years. May be caused due to various reasons such as infection, allergy, lack of oxygen, and inflammatory bowel disease. Abdominal pain, cramping, diarrhea, and fever are common symptoms. Treatment depends on the type of colitis and the symptoms.
Colitis has several causes:
- Infections: Bacterial, viral or parasitic
- Inflammatory bowel disease (like Crohn’s disease and ulcerative colitis)
- Insufficient blood supply (causes ischemic colitis)
- Allergic reactions
- Radiation therapy
Symptoms may vary depending on the severity and cause.
Some symptoms are:
- Abdominal pain
- Cramping
- Diarrhea, with or without blood in the stool (one of the hallmark symptoms of colitis)
- Fever
- Chills
- Fatigue
- Dehydration
- Inflammation in the eyes
- Swelling in the joints
- Canker sores
- Skin inflammation
Treatment depends on the type of colitis and the symptoms:
Infection-associated colitis may be treated with antibiotics, some of the bacterial infection is clostridium difficile and salmonella. Ischemic colitis is treated with intravenous fluid. If there are blood clots surgery may be required.
Medication:
- Anti-inflammatory drugs: Reduce inflammation and discomfort. Balsalazide · Mesalamine · Olsalazine · Sulfasalazine
- Analgesics: To relieve pain. Acetaminophen · Ibuprofen
- Antidiarrheal agents: To control diarrhea. Loperamide
Medical procedures:
Gastrointestinal surgery
Ulcerative colitis:
Causes:
The exact reason for ulcerative colitis is unknown.
A few associated causes are:
- Food habits
- Stress
- Poor immune system
- Family history
Very common (More than 500,000 cases per year in Canada). Treatments can help manage the condition, no known cure. Often requires lab tests or imaging. Common for ages 18-35. Family history may increase the likelihood. Urgent medical attention is recommended.
Symptoms:
-
- Stomach pain and cramping
- Rectal pain
- Joint pain
- Frequent loose bowels
- Rectal bleeding
- Constipation
- Sudden loss of weight
- Fatigue
- Fever
- Common tests & procedures:
Complete blood count (CBC): Hgb levels to check for anemia.
Stool test: To rule out other disease conditions caused by microbes, infections, and parasites.
Colonoscopy: To examine the extent of the damage.
Sigmoidoscopy: To examine the rectum and part of the colon.
X-ray: An abdominal X-ray is taken to identify any puncture in the colon.
CT scan: Provides detailed images of the pelvic region.
Treatments:
Medication
Anti-inflammatory drugs: Reduces inflammation and relieves symptoms.
Sulfasalazine. Olsalazine
Corticosteroids: Relieves symptoms.
Immunomodulators: Reduces immune system responses that trigger inflammation.
Mercaptopurine. Azathioprine
Nutrition:
Foods to eat:
- Low-fiber foods like potatoes, white rice, and refined pasta
- Dairy products like yogurt milk, and cottage cheese
- Foods rich in omega-3 fatty acids like walnuts, salmon, and mackerel
Foods to avoid:
- Caffeine-laden food like tea and coffee
- Alcoholic drinks
- Carbonated drinks
- Foods rich in fiber dried beans, fruits, whole grains, berries, peas, and legumes
- Foods rich in sulfur or sulfites wheat pasta, bread, peanuts, raisins, and cured meats
- Spicy and fatty food
Personal Notes:
As you can see these are very similar as far as symptoms, diagnosis, and treatment. One of the reasons I am writing about colitis is because I have a friend who suffers from this disease. I see the pain and the discomfort he has to go through. We will be getting more into depth further on in this article.
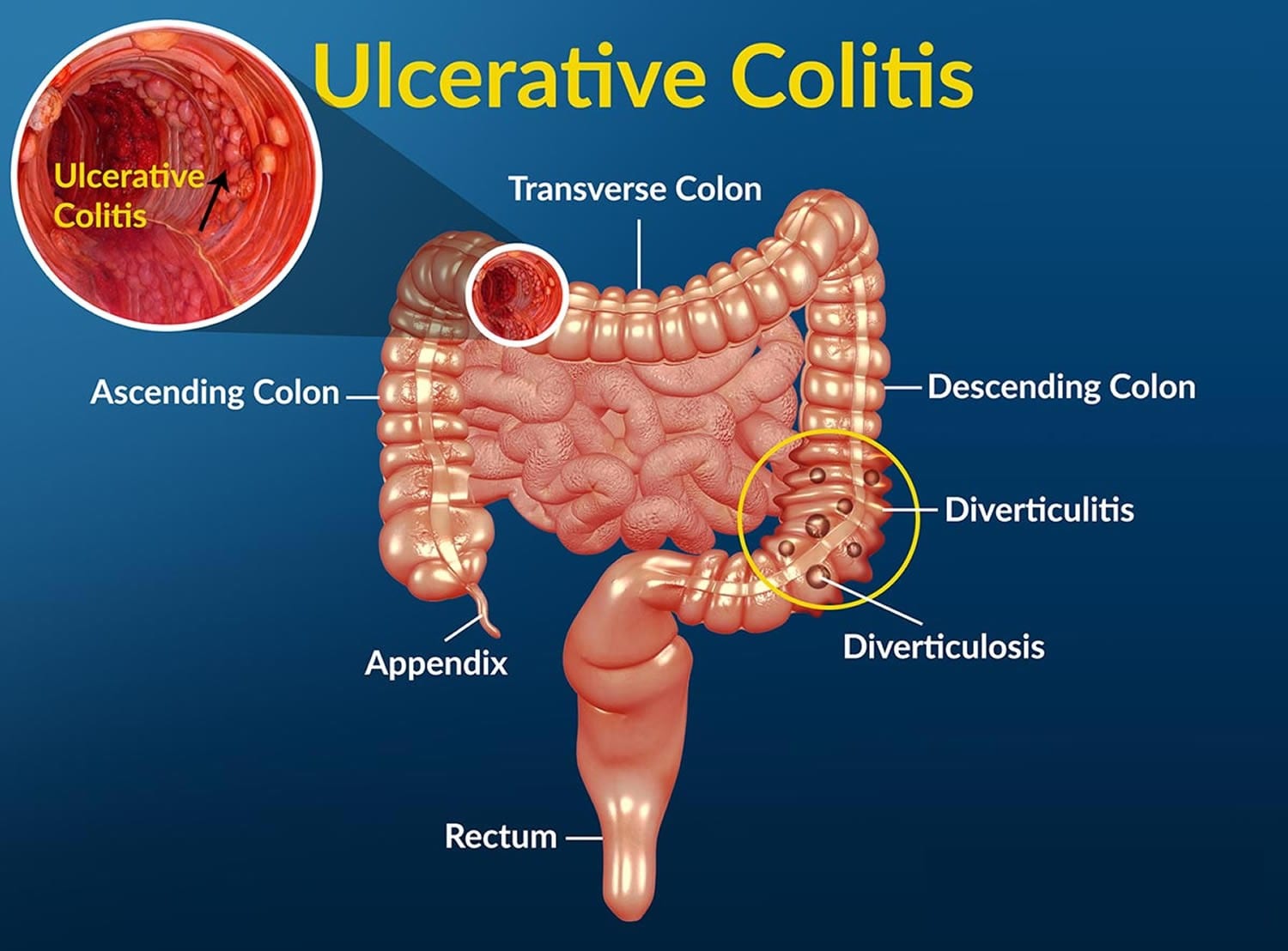
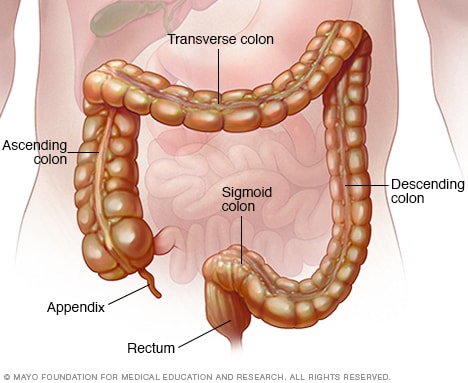
Colitis and the anatomy of the colon:
The colon, or large intestine, is a hollow, muscular tube that processes waste products of digestion from the small intestine, removes water, and ultimately eliminates the remnants as feces (stool) through the anus. The colon is located within the peritoneum, the sac that contains the intestine, located in the abdominal cavity.
The colon is surrounded by many layers of tissue. The innermost layer of the colon is the mucosa that comes into contact with the waste products of digestion. The mucosa absorbs water and electrolytes back into the blood vessels that are located just below the surface in the submucosa. This is surrounded by a circular layer of muscles and then another outer layer of longitudinal muscles that run along the length of the colon. The muscles work together to rhythmically squeeze liquid waste from the cecum through the entire length of the colon. Water is gradually removed, turning the waste into a formed stool so that it is excreted out of the anus in solid form.
The colon frames the organs within the peritoneum, and its segments are named based on their location.
- The colon usually begins in the right lower quadrant of the abdomen, where the terminal ileum, the last part of the small intestine, attaches to the cecum, the first segment of the colon. The appendix is attached to the cecum.
- The ascending colon begins at the cecum and arises from the right lower abdomen to the right upper abdomen near the liver.
- The colon then makes a sharp left turn called the hepatic flexure (hepatic=liver), and is referred to as the transverse colon, as it makes its way to the left upper quadrant of the abdomen near the spleen.
- There is a sharp downward turn called the splenic flexure, and it is referred to as the descending colon as it runs from the left upper quadrant to the left lower quadrant of the abdomen.
- When it descends into the pelvis, it is referred to as the sigmoid colon.
- The last several centimeters of the colon is referred to as the rectum.
- The anus is the final portion of the colon.
Infectious causes of colitis:
Many bacteria reside in the colon; they live in harmony with the body and cause no symptoms. However, some infections can result if a virus, bacteria, or parasite invades the small and/or large intestine.
Common bacteria that cause colitis include:
- Campylobacter,
- Shigella,
- E. Coli,
- Yersinia,
- Salmonella.
These infections usually occur because the patient has eaten contaminated food. Symptoms can include diarrhea with or without blood, abdominal cramps, and dehydration from water loss because of numerous watery, bowel movements. Other organs can also be affected by the infection or the toxins that the bacteria can produce.
Clostridium difficile, commonly referred to as C. diff, is a bacterial cause of colitis that often occurs after a person has been prescribed an antibiotic or has been hospitalized. C. diff is found in the colon of healthy people and coexists with other “normal” bacteria. But when antibiotics are prescribed, susceptible bacteria in the colon can be destroyed, allowing the clostridia to grow unchecked, causing colitis. Patchy membranes form over the colon mucosa and some health care professionals refer to colitis as pseudomembranous colitis.
The bacteria also may be found on many surfaces in the hospital (for example, bedrails, toilets, and stethoscopes), and the infection may spread from person to person (it is highly contagious). Unfortunately, this infection is becoming more common outside the hospital environment, and people can develop community-acquired C. diff colitis without exposure to antibiotics or a medical facility.
Worldwide, the most common parasite infection to cause colitis is Entamoeba histolytica. It is acquired by drinking infected water and can also be passed from person to person because of poor sanitation and hygiene.
Ischemic causes of colitis:
The colon can be thought of as a hollow muscle. It requires a normal blood supply to deliver oxygen and nutrients for the muscle to function normally. When the colon loses its supply of blood and becomes ischemic (isch= restricted + emia=blood supply), it may become inflamed. Ischemia or lack of blood supply causes inflammation of the colon leading to pain, fever, and diarrhea (bowel movements may contain blood).
- As a person ages, the arteries that supply blood to the colon gradually narrow and can cause ischemic colitis. Risk factors for narrowed arteries are the same as atherosclerotic heart disease, stroke, and peripheral artery disease (PAD). These include diabetes, high blood pressure, high cholesterol, and smoking.
- Ischemia caused by low blood pressure or anemia (low red blood cell count) can decrease oxygen delivery to the colon.
- Patients who have atrial fibrillation (AFib) and are not anticoagulated are at risk of developing ischemic bowel. Small blood clots can form in the heart and embolize (travel) to block arteries that supply the colon with blood. This is the same mechanism that can cause a stroke in patients with AFib.
- The blood supply to the colon may be compromised when blood vessels are mechanically obstructed, for example by a twisting of the bowel (volvulus) or a herniation of the colon through openings in the abdomen wall (an incarcerated hernia).
Inflammatory bowel disease (IBD) and colitis:
Ulcerative colitis and Crohn’s disease are the two types of inflammatory bowel disease (IBD) that cause colitis. Crohn’s disease and ulcerative colitis are considered autoimmune diseases (the body’s immune system “attacks” itself).
- Ulcerative colitis always begins in the rectum and may spread to the rest of the colon, spreading from the rectum to the sigmoid, descending, transverse, and finally the ascending colon and cecum in that order. Ulcerative colitis is considered an autoimmune disease, and symptoms include abdominal pain, and bloody, diarrheal bowel movements.
- Crohn’s disease may occur anywhere in the gastrointestinal tract (GI), including the esophagus, stomach, small intestine, and colon. In Crohn’s disease, there may be “skip lesions,” that is, abnormal segments of the GI tract interspersed with normal segments.
Both Crohn’s disease and ulcerative colitis may have other organ systems involved in addition to the gastrointestinal tract.
Microscopic colitis
There are two types of microscopic colitis:
1) collagenous colitis
2) lymphocytic colitis.
Either collagen or lymphocytes (a type of white blood cell) infiltrate into the layers of the wall of the colon, presumably as a result of inflammation. This is an uncommon illness and may be an autoimmune disease. The diarrhea is often watery, and no blood is present in the stool.
Allergic colitis in infants:
In infants younger than 1 year of age, colitis is often due to allergies to cow or soy milk. Allergic colitis may be seen in breastfed babies, where mothers drink cow’s milk and pass that protein into their breast milk.
Pain from inflammation:
Inflammation of the colon causes the muscle layers to go into intermittent spasms, causing colicky or cramp-like pain that comes and goes. The pain is usually in the lower abdomen but can be felt anywhere along the course of the colon. Since the muscles fail to contract in a normal pattern and the colonic contents move through the colon rapidly, there is little opportunity for water to be reabsorbed. This leads to watery diarrhea. If the lining of the colon becomes inflamed and breaks down, bleeding may occur. In ulcerative colitis, small ulcers form and are the cause of bleeding.
Pain before, during, and/or after an episode of diarrhea.
With colitis, particularly colitis involving the distal colon (rectum and sigmoid colon), the pain often crescendos and precedes a diarrheal bowel movement. After the bowel movement, the pain may subside but then return with the next episode of diarrhea. The person also may have a feeling of urgency to have a bowel movement.
Other symptoms of colitis:
Depending upon the cause of the colitis, other organ systems in the body may be involved and produce symptoms such as:
- fever,
- chills,
- malaise,
- fatigue,
- dehydration. (Symptoms of dehydration include weakness, lightheadedness, and decreased urine output.)
Both ulcerative colitis and Crohn’s disease may have associated symptoms outside of the colon due to the body itself attacking other organs. These may include
- joint swelling,
- eye inflammation (iritis),
- canker sores in the mouth (aphthous ulcer),
- skin inflammation (pyoderma gangrenosum).
When should someone contact a doctor about colitis?
Diarrhea is a common sign of colitis. It is usually self-limited and resolves on its own with supportive care, including rest and a short course of a clear-fluid diet. However, seek medical care if diarrhea persists for more than two to three weeks, if there is blood in the stool, fever, or if the person has signs of dehydration.
- Blood in the stool is never normal and should always be evaluated. Common causes of blood in the stool include hemorrhoids; however, other serious causes of bleeding need to be investigated. Colitis is not the only cause of rectal bleeding. Other causes include diverticular disease of the colon (diverticulitis), colon polyps, anal fissures, and cancer.
- Chronic diarrhea may lead to dehydration and changes in the electrolyte balance in the body. If it is severe enough, the dehydration may require treatment with IV fluids or oral rehydration therapy. The symptoms of dehydration may include
- lightheadedness (dizziness), especially when changing from a sitting or lying position to a standing position (orthostatic hypotension);
- weakness;
- dry mouth;
- dry eyes;
- decreased output of urine.
- High fever associated with diarrhea may be a warning sign that a significant infection may be present.
- Abdominal pain is not normal, and while diarrhea may be associated with mild cramps, the presence of increasing abdominal pain requires the need to seek prompt medical attention.
- lightheadedness (dizziness), especially when changing from a sitting or lying position to a standing position (orthostatic hypotension);
What is the treatment for colitis?
The treatment of colitis depends upon the cause.
For undiagnosed or uncontrolled colitis, the initial therapy (regardless of the cause) is to stabilize the patient’s vital signs and help control pain if needed. Rehydration may be accomplished by mouth. However, for those patients who are markedly dry, who are unable to tolerate fluids by mouth, or who have electrolyte abnormalities, intravenous fluids may be required.
Medications are often used to control IBD and the choice of medication is tailored to the individual patient.
Antibiotics are not commonly used unless a specific bacterium is isolated and treatment is known to shorten the course of the infection.
Over-the-counter medications to treat diarrhea should be used with caution, especially if abdominal pain and fever are present. It is always wise to check with a care provider or pharmacist prior to taking antidiarrheal medications.
Surgery is usually not a treatment option for most causes of colitis.
What foods help soothe colitis flares?
Colitis is often associated with diarrhea, and the body can lose significant amounts of fluid with each episode of diarrhea. Moreover, the colon is inflamed, and it is important to try to “rest” it. Since clear fluids tend to be absorbed mostly in the stomach and small intestine, initially avoiding solid foods and promoting a clear fluid diet may be of help in rehydrating the body and resting the colon.
Changing your diet to reduce symptoms or flares may help soothe the symptoms of the disease, but there is no cure for some forms of colitis.
What foods should I avoid if I have colitis?
Depending on the cause, some people with colitis may find that certain foods bring on or make their symptoms worse. Keeping a food diary may be helpful and then avoid foods that may be associated with worsening symptoms.
The Crohn’s & Colitis Foundation of America recommends avoiding the following foods if you have colitis:
- Greasy or fried foods
- Milk or products containing milk
- Certain high-fiber foods like popcorn, seeds, nuts, and corn
People who are lactose intolerant should avoid dairy products containing lactose. There are a variety of companies (for example, Lactaid and Green Valley Organics) that offer lactose-free products such as milk, yogurt, ice cream, and cottage cheese.
What is the prognosis for a person with colitis?
Patients with infectious diarrhea tend to get better relatively quickly with supportive care. Most infections will resolve with or without specific treatment and often do not require antibiotics. Those decisions depend on the patient’s diagnosis.
Patients with inflammatory bowel disease probably will require lifelong treatment to help control their symptoms. The goal, as with any long-term illness, is to allow the patient to live a normal life with minimal symptoms of the disease.
Patients with ischemic colitis need to minimize their risk factors for the progressive narrowing of the arteries. These are the same risks as heart disease and require the same treatment approach, including controlling high blood pressure, diabetes, high cholesterol, and smoking cessation. Patients with severe ischemia that leads to a dead (gangrenous) colon require surgery to remove the gangrenous segment.
Ulcerative Colitis:
Overview:
Gastroenterology & GI Surgery Blog
Ulcerative colitis is an inflammatory bowel disease (IBD) that causes long-lasting inflammation and ulcers (sores) in your digestive tract. Ulcerative colitis affects the innermost lining of your large intestine (colon) and rectum. Symptoms usually develop over time, rather than suddenly.
Ulcerative colitis can be debilitating and can sometimes lead to life-threatening complications. While it has no known cure, treatment can greatly reduce the signs and symptoms of the disease and even bring about long-term remission.
Symptoms:
Ulcerative colitis symptoms can vary, depending on the severity of inflammation and where it occurs. Signs and symptoms may include:
- Diarrhea, often with blood or pus
- Abdominal pain and cramping
- Rectal pain
- Rectal bleeding — passing a small amount of blood with stool
- Urgency to defecate
- Inability to defecate despite urgency
- Weight loss
- Fatigue
- Fever
- In children, failure to grow
Most people with ulcerative colitis have mild to moderate symptoms. The course of ulcerative colitis may vary, with some people having long periods of remission.
Types:
Doctors often classify ulcerative colitis according to its location. Types of ulcerative colitis include:
- Ulcerative proctitis. Inflammation is confined to the area closest to the anus (rectum), and rectal bleeding may be the only sign of the disease. This form of ulcerative colitis tends to be the mildest.
- Proctosigmoiditis. Inflammation involves the rectum and sigmoid colon (lower end of the colon). Signs and symptoms include bloody diarrhea, abdominal cramps and pain, and an inability to move the bowels in spite of the urge to do so (tenesmus).
- Left-sided colitis. The inflammation extends from the rectum up through the sigmoid and descending colon. Signs and symptoms include bloody diarrhea, abdominal cramping pain on the left side, and unintended weight loss.
- Pancolitis. Pancolitis often affects the entire colon and causes bouts of bloody diarrhea that may be severe, abdominal cramps and pain, fatigue, and significant weight loss.
- Acute severe ulcerative colitis. This rare form of colitis affects the entire colon and causes severe pain, profuse diarrhea, bleeding, fever, and inability to eat.
When to see a doctor:
See your doctor if you experience a persistent change in your bowel habits or if you have signs and symptoms such as:
- Abdominal pain
- Blood in your stool
- Ongoing diarrhea that doesn’t respond to over-the-counter medications
- Diarrhea that awakens you from sleep
- An unexplained fever lasting more than a day or two
Although ulcerative colitis usually isn’t fatal, it’s a serious disease that, in some cases, may cause life-threatening complications.
Causes
The exact cause of ulcerative colitis remains unknown. Previously, diet and stress were suspected, but now doctors know that these factors may aggravate but don’t cause ulcerative colitis.
One possible cause is an immune system malfunction. When your immune system tries to fight off an invading virus or bacterium, an abnormal immune response causes the immune system to attack the cells in the digestive tract, too.
Heredity also seems to play a role in that ulcerative colitis is more common in people who have family members with the disease. However, most people with ulcerative colitis don’t have this family history.
Risk factors:
Ulcerative colitis affects about the same number of women and men. Risk factors may include:
- Age. Ulcerative colitis usually begins before the age of 30. But, it can occur at any age, and some people may not develop the disease until after age 60.
- Race or ethnicity. Although whites have the highest risk of the disease, it can occur in any race. If you’re of Ashkenazi Jewish descent, your risk is even higher.
- Family history. You’re at higher risk if you have a close relative, such as a parent, sibling, or child, with the disease.
Complications:
Possible complications of ulcerative colitis include:
- Severe bleeding
- A hole in the colon (perforated colon)
- Severe dehydration
- Liver disease (rare)
- Bone loss (osteoporosis)
- Inflammation of your skin, joints, and eyes
- An increased risk of colon cancer
- A rapidly swelling colon (toxic megacolon)
- Increased risk of blood clots in veins and arteries
Always see your Doctor First!!!
Effective Home Remedies For Ulcerative Colitis Symptoms
Oftentimes, conventional ulcerative colitis treatment involves either surgery or drug therapy, and anti-inflammatory drugs are often the initial step of the treatment process. There are two common anti-inflammatory medications that are often prescribed for people having ulcerative colitis, which are corticosteroids and aminosalicylates. However, these medications also expose you to some side effects. Thus, it is important to look for some natural ways to solve your problem without the use of harmful drugs.
Here, we will uncover top natural but effective home remedies for ulcerative colitis symptom removal that you can easily apply without complicated preparation.
1. Turmeric
This is an Indian spice used in curry and also one of the must-try home remedies for ulcerative colitis. This is thanks to the curcumin compound which is an antioxidant and has anti-inflammatory properties. A study showed that this phytochemical if combined with mesalamine therapy, was superior to placebo in inducing the endoscopic and clinical remission in sufferers of mild-to-moderate ulcerative colitis. Some ways that turmeric’s pharmacological properties benefit ulcerative colitis are: It modulates the release of some inflammatory agents causing ulcerative colitis. It alleviates the symptoms of this condition like mucosal ulceration and thickening of intestinal walls. It has gastroprotective properties and immunomodulatory action improves antioxidant effects and protects from gastric infections.
Warnings:
- If you are considering taking turmeric supplements, consult your doctor first.
- Turmeric supplements should be avoided if you are using blood thinners or having gall bladder obstructions.
- Also, consult your doctor if you have a bleeding disorder.
- Women who are pregnant and breastfeeding should not use this ingredient.
- Stop using turmeric supplements about 2 weeks before surgery.
- Turmeric might interact with specific medications such as diabetes, stomach acid-reducing drugs, and blood thinners.
- Limit your intake of turmeric as a spice if you have kidney stones or gout.
Gingko Biloba is one of the oldest living tree species which has a long history of use in dealing with blood disorders and memory problems. This herb is even good for people with ulcerative colitis. The leaves of ginkgo contain flavonoids and terpenoids, which are antioxidants. It has been shown to be effective in treating experimental colitis in rodents.
3. Boswellia
This is a medicinal herb that originated from a tree native to India. The resin of the bark has an active ingredient that is believed to possess anti-inflammatory effects. In the extract form, it is popularly used to deal with inflammatory conditions like rheumatoid arthritis.
According to a study, it was found that 82% of people taking 350 mg of a Boswellia extract 3 times per day had remission from mild-to-moderate ulcerative colitis.
In reality, Boswellia is available in the pill form. Standardly, it has 60% of Boswellia acids.
Notes: Boswellia extract should not be used for over 12 weeks if not under the supervision of a doctor.
4. Bromelain
This is a mixture of protein-digesting enzymes originating from the pineapple stem. Bromelain is believed to decrease digestive inflammation. In accordance with a Duke University animal study, it was found that daily treatment with oral bromelain reduces the risk and severity of colitis.
Taking bromelain extract or dietary supplements is said to be more efficient than consuming fresh pineapples in reducing inflammation and pain.
The daily dose of bromelain is 3-4 doses of 40mg or about 2 standard-size slices of pineapple. Commercial preparations of bromelain are available in capsule, tablet, and liquid form. However, as these products have mostly stem bromelain, the dosing of each is different. The majority of manufacturers recommend taking 500-1000 mg of bromelain each day.
Notes:
- Bromelain might increase heart rate, trigger allergic reactions, and cause diarrhea or vomiting in some people.
- Women taking this substance might experience increased menstrual bleeding.
- People with liver disease, kidney disease, high blood pressure, or a bleeding disorder should be cautious when using bromelain.
5. Probiotics
Regarding home remedies for ulcerative colitis, probiotics are believed to be good for managing ulcerative colitis as well as other chronic digestive disorders.
They are considered friendly bacterial agents that can control harmful bacteria whilst decreasing inflammation and boosting the protective mucus lining of the gut. Furthermore, they are reckoned as safe with no side effects.
The University of Alberta study showed that probiotics can restore and maintain a natural microbial flora in the gut. It decreases harmful inflammatory responses and maintains remission. Certainly, probiotics are not a replacement for conventional medication, but they could support the treatment process significantly.
You can find probiotics in yogurt and kefir. It is also available in capsule form. Actually, there is no regulation of probiotics in the food form. But, you should discuss with your doctor if you are using any complementary remedies.
6. Aloe Vera.
Studies have found that aloe vera has the ability to treat mild to moderate cases of ulcerative colitis because of its anti-inflammatory properties.
This herbal therapy is widely used to treat IBD. In fact, aloe vera gel can inhibit the production of various inflammatory agents and can provide therapeutic benefits for IBD sufferers.
There is no specific dosage of aloe vera for ulcerative colitis. But, you should take 100ml of aloe vera juice twice per day for about 4 weeks to improve the symptoms of this condition and increase the chances for remission. However, in general, the quantity had better be based on your age as well as the condition’s severity.
Notes:
- The topical use of aloe vera gel does not come with side effects.
- If taken internally, people with Crohn’s disease, kidney disease, hemorrhoids,
Psyllium is a plant that contains seeds and husks. Husks are an outer coating of the seeds of the psyllium plant. Both the husk and seed powder are important for ulcerative colitis treatment, but husk powder seems to be more important. Psyllium is a rich source of fiber acts as a sponge and absorbs toxins within the digestive tract. It also helps eliminate toxins when it travels to the colon.
Furthermore, this ingredient can enhance your gut motility, lessen constipation symptoms, and improve the eradication of waste.
You can take a mixture of psyllium husk/seed powder every day to reap its benefits for ulcerative colitis. But, use organic psyllium because psyllium tends to be contaminated with pesticides.
What you have to do is:
- Buy organic psyllium husk powder and psyllium seed powder
- Mix them together with a ratio of 1:1
- Add water and drink it
Notes: It is still better to discuss with your doctor whether or not psyllium is appropriate for your own case.
8. Olive Oil
Olive oil is one of the most efficient home remedies for ulcerative colitis, in both mild and moderate cases. Having a high content of mono-unsaturated fats, olive oil also possesses immunomodulatory along anti-inflammatory properties.
Andrew Hart, MD, of the University of East Anglia in Norwich, England has said that consuming large amounts of oleic acid (from 2-3 tablespoons of olive oil) could prevent the risk of ulcerative colitis by half. Oleic acids can dampen down bowel inflammation by blocking chemicals that stimulate inflammation.
Just simply consume 2-3 tablespoons of extra virgin olive oil every day to take advantage of it for ulcerative colitis relief.
Wheatgrass is biologically referred to as Triticum aestivum. This is a young wheat plant and its cotyledons are used to make powders, juices, and other supplements.
Wheatgrass has a number of health benefits due to its main reviving properties. It is often used to treat nausea, bowel problems, constipation, acidity, high blood pressure, etc. It can promote weight loss, help detoxify the body, and be used for oral care.
In regard to treating ulcerative colitis, wheatgrass is touted as a natural food improving symptoms of this condition.
Many studies have been conducted on the use of wheatgrass juice for relieving ulcerative colitis.
Possibly being an autoimmune disease, wheatgrass is claimed to help patients with ulcerative colitis because it acts as a strong immune modulator.
You can drink 4 teaspoons of wheatgrass juice every day, then steadily increase that dosage to 3.5 ounces each day to get the best results.
Notes:
- Consult your doctor before using this plant. It is just a complementary treatment, not an alternative for treating ulcerative colitis.
- People with gluten intolerance and allergies to wheat or grass products or having celiac disease have to avoid consuming wheatgrass.
10. Fish Oil
Due to omega-3 fatty acid content plus anti-inflammatory properties, fish oil can relieve symptoms of active ulcerative colitis. The omega-3 fatty acids are polyunsaturated fatty acids that could decrease inflammation.
The researchers at Boston University Medical Center showed that sufferers of gastrointestinal disorders may have abnormal profiles of essential fatty acids. The EPA in fish oil interferes with the synthesis of highly inflammatory leukotriene B4 in the lining of the colon and this impact contributes to the improvement of ulcerative colitis.
Thus, a remedy using fish oil can help with ulcerative colitis relief. You can start by taking 1 gram of fish oil supplement every day, then increase steadily to 2-4 grams.
11. Slippery Elm
Slippery elm bark powder coats and soothes the alimentary canal and digestive tract which are inflamed and ulcerated as the result of ulcerative colitis, IBS, Crohn’s disease, and IBD. It is thanks to the mucilage content. Also, it can add bulk to the stool to decrease diarrhea.
What you need to do is:
Method 1:
- Mix 1 tablespoon of powdered slippery elm bark with 1 cup of hot water
- Allow it to steep for several minutes
- Have it twice per day
Method 2:
- Mix 1 teaspoon of sugar with the same amount of slippery elm together
- Add them to 2 cups of hot water to create a gruel
- Have it twice per day
12. Calendula
Calendula is a common plant in North America and Europe and has been used as an herbal medicine for centuries. Calendula has anti-inflammatory and soothing properties, which are effective in treating ulcerative colitis. It also improves digestion and boosts tissue healing.
- Put 1-2 teaspoons of calendula flowers in a cup of hot water
- After allowing it to steep for 15 minutes or so, strain it
- Have this solution 2-3 times per day
13. Fenugreek.
Among home remedies for ulcerative colitis, fenugreek is easy to find. This plant forms a defensive coat along the digestive tract. Furthermore, it also alleviates inflammation and provides you with nutrition, like vitamins A and C, calcium, iron, protein, and other nutrients.
What you need to do is:
- Add 1 teaspoon of crushed fenugreek seeds into a cup of hot water
- Allow it to steep for 4-5 minutes
- Have this tea every day till you see good results
14. Ginger
This spice is used for a variety of natural treatments for infections and other related problems. The anti-inflammatory effects and a rich source of antioxidants in ginger make it one of the best home remedies for ulcerative colitis symptoms. It can not only remove harsh chemicals within the body while improving the digestive tract. You should not take it in excess, however. All you have to do is:
Mix 2 tablespoons of grated ginger with 1 cup of water boil it up and allow it to simmer for 10 minutes. Add lemon juice and honey for taste (optional) Strain the tea and have it do this several times per week to get good results or, you can take ginger supplements with the supervision of a doctor.
15. Cabbage Juice
This is a wonderful remedy for ulcerative colitis due to its sufficient content of minerals and nutrients for the inner bowel’s health. At the same time, it also helps reduce inflammation. Blend some cabbage in a blender to take its juice. Drink the juice regularly to reduce the symptoms of ulcerative colitis
16. Buttermilk
Often used for curing ulcerative colitis, buttermilk can also aid in preventing constipation and promoting bowel movement. Furthermore, it reduces the inner inflammation that has impacted the rectum and colon. You just need to drink buttermilk a few times per day to relieve this condition.
17. Green Tea
In green tea, there is epigallocatechin Gallate (EGCG) which has anti-inflammatory and antioxidant effects, thereby improving cardiovascular health. Also, it plays an important role in preventing and treating cancer. Moreover, many recent studies have proved that this extract possesses a positive effect on people with bowel diseases like ulcerative colitis.
A study conducted at the University of Kentucky assessed the effectiveness and safety of an oral dose of green tea polyphenols in sufferers with mild-to-moderate ulcerative colitis. It was shown that 85% of people involved in the polyphenol group had remission as opposed to the ones in the placebo group. After all, whether or not you are affected by ulcerative colitis, it might be wise to stock up on green tea because it offers a host of many health benefits.
18. Chamomile
It could be beneficial as it can soothe the digestive tract and has anti-inflammatory properties. Chamomile may relieve cramping as well as irritation of the intestines keeping the ulcers from developing and boosting their healing if they have progressed. You can take the steps here to make use of this herb for ulcerative colitis:
Add 3 teaspoons of dried chamomile flowers to a cup of hot water, let it steep for 10 minutes, and strain it. Have it 3 times per day, especially during flare-ups.
Notes: Do not use chamomile on an ongoing basis. Avoid it entirely if you are allergic to ragweed.
19. Licorice Drinking
Licorice root tea is one of the most effective home remedies for ulcerative colitis because it helps soothe the pain associated with this condition. To prepare the tea, you can take the following steps.
Boil ½ ounce of licorice root in about 2 cups of water. After 15 minutes of steeping, strain, and drink it. You can also find licorice in the form of tablets or extracts.
Add Omega-3 Fatty Acids to your diet, as part of a healthy diet, healthy fats which are found in foods such as fatty fish can keep inflammation under control and relieve ulcerative colitis symptoms. In fact, omega-3 fats are good for sufferers of both Crohn’s and ulcerative colitis because of their strong anti-inflammatory ability. This effect can fuel the cells lining the intestinal tract.
Home Remedies For Ulcerative Colitis
Reduce the consumption of dairy products. Take protein and vitamin C supplements. Drink enough water and consume liquids. Exercise regularly and practice stress-relieving techniques.
Stop smoking plus alcohol consumption. Avoid processed food, carbonated drinks, meat, and caffeine. Avoid eating large meals.
In addition to these remedies, you need also to take some preventative measures and carry out some dietary changes to keep your problem at bay. Besides, it is not necessary to say that you need to consult your doctor once the symptoms get worse.
Personal Notes:
I hope the home remedies will help you. I am not a fan of, “Big Pharma” but I realize some medications are necessary for proper treatment methods.
Thank you for reading.
Michael.
Comments are welcome.

Thanks a lot for such an amazing review about SYMPTOMS COLITIS, ULCERATIVE COLITIS!
I have been searching for an article for a long time about this but I did not find much on the internet and if I found it was very poorly explained. I will take more care of my body after reading this.If you don’t mind, I will share this article on my social media account.
Thanks again and keep in touch!
Hi Razvanllie,
Thank you for your comments. Honesty is very important to me. I certainly would appreciate your help in sharing this article and helping someone out. I look at my traffic everyday to see if my message is getting through. I spend a lot of time on research to offer help for free.
Best wishes,
Michael
Hello, I really want to first appreciate your effort in putting this great website together and writing this article. even without going to medical school, with your explicit explanation, anyone can fully understand the entire article. i am glad you are bringing this to light. thank you once again for this post
Hi Benny,
Thank you for your comments. It is all about trying to help someone who may be in pain, and instead of going through the high cost of prescription medications, perhaps trying some home remedies.
Best wishes,
Michael