What is Influenza?
Blue indicates link
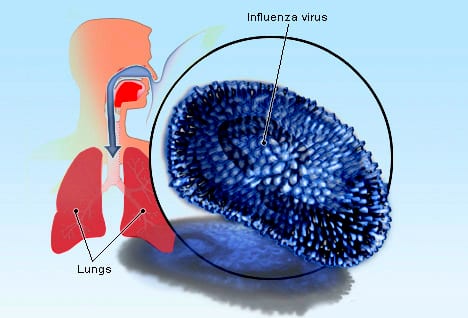
Three of the four types of influenza viruses affect humans: Type A, Type B, and Type C. Type D has not been known to infect humans but is believed to have the potential to do so. Usually, the virus is spread through the air from coughs or sneezes. This is believed to occur mostly over relatively short distances. It can also be spread by touching surfaces contaminated by the virus and then touching the mouth or eyes. A person may be infectious to others both before and during the time they are showing symptoms.
The infection may be confirmed by testing the throat, sputum, or nose for the virus. A number of rapid tests are available; however, people may still have the infection even if the results are negative.
Influenza spreads around the world in yearly outbreaks, resulting in about three to five million cases of severe illness and about 250,000 to 500,000 deaths. About 20% of unvaccinated children and 10% of unvaccinated adults are infected each year. In the northern and southern parts of the world, outbreaks occur mainly in the winter, while around the equator, outbreaks may occur at any time of the year. Death occurs mostly in the young, the old, and those with other health
problems. Larger outbreaks known as pandemics are less frequent. In the 20th century, three influenza pandemics occurred: Spanish influenza in 1918 (40–50 million deaths), Asian influenza in 1957 (two million deaths), and Hong Kong influenza in 1968 (one million deaths). The World Health Organization declared an outbreak of a new type of influenza A/H1N1 to be a pandemic in June 2009. Influenza may also affect other animals, including pigs, horses, and birds.
Global influenza pandemic:
The world will face another influenza pandemic – the only thing we don’t know is when it will hit and how severe it will be. Global defenses are only as effective as the weakest link in any country’s health emergency preparedness and response system.
WHO is constantly monitoring the circulation of influenza viruses to detect potential pandemic strains: 153 institutions in 114 countries are involved in global surveillance and response.
Every year, the WHO recommends which strains should be included in the flu vaccine to protect people from seasonal flu. In the event that a new flu strain develops pandemic potential, WHO has set up a unique partnership with all the major players to ensure effective and equitable access to diagnostics, vaccines, and antivirals (treatments), especially in developing countries.
According to new estimates published today, between 291,000 and 646,000 people worldwide die from seasonal influenza-related respiratory illnesses each year, higher than a previous estimate of
250,000 to 500,000 and based on a robust, multinational survey. (Survey conducted Dec 13, 2017)
Global flu surveillance protects all nations, including the U.S.
CDC works with global partners to improve worldwide capacity for influenza prevention and control. CDC has helped more than 60 countries build surveillance and laboratory capacity to rapidly detect and respond to influenza threats, including viruses with the potential to cause global pandemics. These efforts, along with technical support, have helped some partners generate estimates of influenza-associated deaths, which contributed to this global effort.
Global surveillance also provides the foundation for selecting the viruses used to make seasonal flu vaccines each year. This helps improve the effectiveness of flu vaccines used in the United States. Global surveillance also is crucial to pandemic preparedness by identifying viruses overseas that might pose a human health risk to people in the United States.
“This work adds to a growing global understanding of the burden of influenza and populations at highest risk,” says CDC researcher Danielle Iuliano, lead author of The Lancet study. “It builds the evidence base for influenza vaccination programs in other countries.”
The study authors note that these new estimates are limited to flu-associated respiratory deaths and therefore may underestimate the true global impact of seasonal influenza. Influenza infection can create or exacerbate other health factors which are then listed as the cause of death on death certificates, for example, cardiovascular disease, diabetes, or related complications. Additional research to estimate respiratory causes of flu-associated deaths is ongoing.
Estimates of the number of flu patients who also develop a bacterial infection range from as low as 2 percent to as high as 65 percent, according to one 2016 report. It is estimated that between 70 and 85 percent of seasonal flu-related deaths have occurred in people 65 years and older. (Study did: Nov 19, 2018)
Fragile and vulnerable settings:
More than 1.6 billion people (22% of the global population) live in places where protracted crises (through a combination of challenges such as drought, famine, conflict, and population displacement) and weak health services leave them without access to basic care.
Fragile settings exist in almost all regions of the world, and these are where half of the key targets in the sustainable development goals, including on child and maternal health, remain unmet.
WHO will continue to work in these countries to strengthen health systems so that they are better prepared to detect and respond to outbreaks, as well as able to deliver high-quality health services, including immunization.
For most people, influenza resolves on its own. But sometimes, influenza and its complications can be deadly. People at higher risk of developing flu complications include:
- Young children under age 5, and especially those under 12 months
- Adults older than age 65
- Residents of nursing homes and other long-term care facilities
- Pregnant women and women up to two weeks postpartum
- People with weakened immune systems
- People who have chronic illnesses, such as asthma, heart disease, kidney disease, liver disease, and diabetes
- People who are very obese, with a body mass index (BMI) of 40 or higher
Though the annual influenza vaccine isn’t 100 percent effective, it’s still your best defense against the flu.
Symptoms
Initially, the flu may seem like a common cold with a runny nose, sneezing, and sore throat. But colds usually develop slowly, whereas the flu tends to come on suddenly. And although a cold can be a nuisance, you usually feel much worse with the flu.
Common signs and symptoms of the flu include:
- Fever over 100.4 F (38 C)
- Aching muscles
- Chills and sweats
- Headache
- Dry, persistent cough
- Fatigue and weakness
- Nasal congestion
- Sore throat
Seasonal influenza is characterized by a sudden onset of fever, cough (usually dry), headache, muscle and joint pain, severe malaise (feeling unwell), sore throat, and a runny nose. The cough can be severe and can last 2 or more weeks. Most people recover from fever and other symptoms within a week without requiring medical attention. However, influenza can cause severe illness or death, especially in people at high risk.
Illnesses range from mild to severe and even death. Hospitalization and death occur mainly among high-risk groups. Worldwide, these annual epidemics are estimated to result in about 3 to 5 million cases of severe illness and about 290,000 to 650,000 respiratory deaths.
In industrialized countries, most deaths associated with influenza occur among people aged 65 or older. Epidemics can result in high levels of worker/school absenteeism and productivity losses. Clinics and hospitals can be overwhelmed during peak illness periods.
The effects of seasonal influenza epidemics in developing countries are not fully known, but research estimates that 99% of deaths in children under 5 years of age with influenza-related lower respiratory tract infections are found in developing countries.
Risk factors
Factors that may increase your risk of developing influenza or its complications include:
- Age. Seasonal influenza tends to target children younger than 12 months of age and adults 65 years old or older.
- Living or working conditions. People who live or work in facilities with many other residents, such as nursing homes or military barracks, are more likely to develop influenza. People who are hospitalized are also at higher risk.
- Weakened immune system. Cancer treatments, anti-rejection drugs, long-term use of steroids, organ transplants, blood cancer, or HIV/AIDS can weaken your immune system. This can make it easier for you to catch influenza and may also increase your risk of developing complications.
- Chronic illnesses. Chronic conditions, including lung diseases such as asthma, diabetes, heart disease, neurological or neurodevelopmental disease, an airway abnormality, and kidney, liver, or blood disease, may increase your risk of influenza complications.
- Aspirin uses underage 19. People who are younger than 19 years of age and receiving long-term aspirin therapy are at risk of developing Reye’s syndrome if infected with influenza.
- Pregnancy. Pregnant women are more likely to develop influenza complications, particularly in the second and third trimesters. Women who are up to two weeks postpartum also are more likely to develop influenza-related complications.
- Obesity. People with a body mass index (BMI) of 40 or more have an increased risk of complications from the flu.
Complications
If you’re young and healthy, seasonal influenza usually isn’t serious. Although you may feel miserable while you have it, the flu usually goes away in a week or two with no lasting effects.
But children and adults at high risk may develop complications such as:
- Pneumonia
- Bronchitis
- Asthma flare-ups
- Heart problems
- Ear infections
Pneumonia is the most serious complication. For older adults and people with a chronic illness, pneumonia can be deadly.
How many people died from flu during the 2017-2018 season?
While flu deaths in children are reported to the CDC, flu deaths in adults are not nationally notifiable. In order to monitor influenza-related deaths in all age groups, the CDC tracks pneumonia and influenza (P&I)-attributed deaths through the National Center for Health Statistics (NCHS) Mortality Reporting System. This system tracks the proportion of death certificates processed that list pneumonia or influenza as the underlying or contributing cause of death. This system provides an overall indication of whether flu-associated deaths are elevated, but does not provide an exact number of how many people died from flu.
During the 2017-2018 season, the percentage of deaths attributed to pneumonia and influenza (P&I) was at or above the epidemic threshold for 16 consecutive weeks. During the past five seasons, the average number of weeks this indicator was above the threshold was 11 (range of 7 to 15 weeks). Nationally, mortality attributed to P&I exceeded 10.0% for four consecutive weeks, peaking at 10.8% during the week ending January 20, 2018.
As it does for the numbers of flu cases, doctor’s visits, and hospitalizations, the CDC also estimates deaths in the United States using mathematical modeling. CDC estimates that from 2010-2011 to 2013-2014, influenza-associated deaths in the United States ranged from a low of 12,000 (during 2011-2012) to a high of 56,000 (during 2012-2013). Death certificate data and weekly influenza virus surveillance information were used to estimate how many flu-related deaths occurred among people whose underlying cause of death on their death certificate included respiratory or circulatory causes.
How effective was the 2017-2018 flu vaccine?
The overall vaccine effectiveness (VE) of the 2017-2018 flu vaccine against both influenza A and B viruses is estimated to be 40%. This means the flu vaccine reduced a person’s overall risk of having to seek medical care at a doctor’s office for flu illness by 40%. Protection by virus type and subtype was: 25% against A(H3N2), 65% against A(H1N1), and 49% against influenza B viruses.
While flu vaccine can vary in how well it works, flu vaccination is the best way to prevent flu and its potentially serious complications and prevents millions of flu illnesses and related doctors’ visits and tens of thousands of hospitalizations. For example, during the 2016–2017 influenza season, CDC estimates that the flu vaccine prevented an estimated 5.3 million illnesses, 2.6 million medical visits, and 85,000 hospitalizations associated with influenza. Similar estimates for 2017-2018 will be released in fall 2018. Influenza vaccination also has been shown to reduce the risk of flu death in children.
Timing of Vaccination
Optimally, vaccination should occur before the onset of influenza activity in the community. Healthcare providers should offer vaccination by the end of October, if possible. Children aged 6 months through 8 years who require 2 doses (see Children Aged 6 Months through 8 Years) should receive their first dose as soon as possible after the vaccine becomes available, to allow the second dose (which must be administered 4 weeks later) to be received by the end of October.
Although some available data indicate that early vaccination (e.g., in July and August) might be associated with sub-optimal immunity before the end of the influenza season, particularly among older adults, the relative contribution of the potential waning of immunity compared with those of other determinants of the impact of vaccination (e.g., timing and severity of the influenza season, the impact of missed opportunities when individuals delay vaccination and fail to return later in the season, and programmatic constraints) is unknown.
Although delaying vaccination might result in greater immunity later in the season, deferral also might result in missed opportunities to vaccinate, as well as difficulties in vaccinating a population within a more constrained time period. Community vaccination programs should balance maximizing the likelihood of persistence of vaccine-induced protection through the season with avoiding missed opportunities to vaccinate. After the onset of influenza, circulation occurs. Revaccination later in the season of persons who have already been fully vaccinated is not recommended.
Vaccination should continue to be offered as long as influenza viruses are circulating and an unexpired vaccine is available. To avoid missed opportunities for vaccination, providers should offer vaccination during routine health care visits and hospitalizations when a vaccine is available. Vaccination efforts should be structured to ensure the vaccination of as many persons as possible before influenza activity in the community begins.
In any given season, the optimal time to vaccinate cannot be predicted precisely because influenza seasons vary in timing and duration. Moreover, more than one outbreak might occur in a given community in a single year. In the United States, localized outbreaks that indicate the start of seasonal influenza activity can occur as early as October. However, in 74% of influenza seasons from 1982–83 through 2015–16, peak influenza activity (which often is close to the midpoint of influenza activity for the season) did not occur until January or later, and in 59% of seasons, the peak was in February or later.
Prevention
The Centers for Disease Control and Prevention (CDC) recommends annual flu vaccination for everyone age 6 months or older.
Each year’s seasonal flu vaccine contains protection from the three or four influenza viruses that are expected to be the most common during that year’s flu season. This year, the vaccine will be available as an injection and as a nasal spray.
In recent years, there was concern that the nasal spray vaccine wasn’t effective enough against certain types of flu. However, the nasal spray vaccine is expected to be effective in the 2019-2020 season. The nasal spray still isn’t recommended for some groups, such as pregnant women, children between 2 and 4 years old with asthma or wheezing, and people who have compromised immune systems.
Most types of flu vaccines contain a small amount of egg protein. If you have a mild egg allergy — you get hives only from eating eggs, for example — you can receive the flu shot without any additional precautions. If you have a severe egg allergy, you should be vaccinated in a medical setting and be supervised by a doctor who is able to recognize and manage severe allergic conditions.
Controlling the spread of infection
The influenza vaccine isn’t 100 percent effective, so it’s also important to take measures such as these to reduce the spread of infection:
- Wash your hands. Thorough and frequent hand-washing is an effective way to prevent many common infections. Or use alcohol-based hand sanitizers if soap and water aren’t readily available.
- Contain your coughs and sneezes. Cover your mouth and nose when you sneeze or cough. To avoid contaminating your hands, cough or sneeze into a tissue or into the inner crook of your elbow.
- Avoid crowds. The flu spreads easily wherever people congregate — in child care centers, schools, office buildings, auditoriums, and public transportation. By avoiding crowds during peak flu season, you reduce your chances of infection. And if you’re sick, stay home for at least 24 hours after your fever subsides so that you lessen your chance of infecting others.
Natural and Herbal Remedies. Please click on the product for a link for the best choices, prices, and fastest delivery.
1. Vitamin C (1,000 mg 3–4x daily)
Vitamin C helps with immune system function and boosts white blood cells. Research shows that vitamin C has shortened the duration of colds and can decrease the number of colds in physically active people.
Take 1,000 milligrams of vitamin C daily to ward off a cold or the flu and up to 4,000 milligrams daily when you are experiencing symptoms. For the most dietary vitamin C, eat whole fruits and vegetables.
2. Vitamin D3 (2,000 IU daily)
Vitamin D is produced in the body by sunlight and regulates the expression of over 2,000 genes, including those of the immune system. Unfortunately, up to 90 percent of people are deficient in vitamin D. Recent research shows that low vitamin D levels are linked to higher rates of cold, flu, and respiratory infections.
Many physicians believe that the current recommended daily amounts of vitamin D are far too low and that 2,000 units rather than 200–400 units per day are a better choice. You can also order home testing kits to test your vitamin D levels.
3. Echinacea (1,000 mg 2–3x daily)
This herb can help your body fight off infections, but it is best to take it at the first sign of illness.
An extract of echinacea was tested in a double-blind, randomized, controlled trial in 2013. Researchers found that the echinacea effectively treated respiratory tract infections in the short- and long-term, and didn’t cause the same resistance as a popular flu medication, oseltamivir often causes when treating this illness.
A randomized, double-blind placebo-controlled study conducted in 2000 indicates that drinking five to six cups of echinacea tea per day as soon as upper respiratory symptoms developed, and reducing the number to one cup of tea over a 5-day period, was effective for relieving cold and flu symptoms.
Echinacea acts as an anti-inflammatory, which can help reduce bronchial symptoms of cold and flu. It directly attacks yeast and other kinds of fungus.
Different preparations have different concentrations of echinacea. Some common preparations and dosages include:
- Tablets containing 6.78 milligrams of echinacea extract, two tablets three times a day
- 900 milligrams of echinacea root tincture daily
- Five to six cups of echinacea tea on the first day of symptoms, and then 1 cup a day thereafter
4. Elderberry (10 mL daily)
It is believed that this herb can deactivate the flu virus and naturally boost immunity. The flowers and berries of elderberry are said to boost the immune system, treat the flu, and relieve sinus pain.
Elderberry does seem to attack flu viruses and reduce bronchial inflammation. A preliminary study found that when 15 milliliters of elderberry syrup was taken four times daily for a five-day period, it relieved symptoms of influenza an average of four days earlier than those taking a placebo.
5. Oregano Oil (500 mg 2x daily)
Oregano oil has a powerful antiviral effect. I like to use oregano oil to fight viral infections and although there aren’t studies evaluating the efficacy of oregano on influenza specifically, there is research that indicates the powerful antiviral properties of the essential oil.
6. Zinc (50–100 mg daily)
Zinc supports immune function and has an antiviral effect. It works best when taken at the first sign of illness. Zinc may lessen the symptoms of the cold virus, but excessive amounts aren’t good for you. Zinc pills and sprays do not seem to be effective.
Take 50–100 milligrams of zinc daily to ward off or treat cold and flu symptoms.
7. Brewer’s Yeast
This popular supplement contains B vitamins, chromium, and protein. It is used for colds, flu, and other respiratory tract infections. In fish, brewer’s yeast stimulates immunity by positively influencing the microbiome, which may also improve digestive function.
Research conducted at the University of Michigan Medical Center found that a yeast supplement was able to reduce cold and flu symptom severity and lead to significantly shorter duration of symptoms in patients.
8. Essential Oils for Flu
Rubbing peppermint and frankincense essential oil into the neck and bottoms of the feet can naturally support the immune system.
I also like to use clove oil to protect my body against infection and speed recovery from the flu. Research confirms that clove oil has antimicrobial and antioxidant properties.
Care for Flu Prevention
During the 1918 flu epidemic, flu patients who received chiropractic care survived much more readily than those who didn’t. This is because chiropractic care focuses on the health of your nervous system, which can help to boost your immunity.
A 2011 study showed some promise for chiropractic adjustments and their potential to help boost the immune system.
10. Probiotics
Restoring the beneficial bacteria in your gut can help boost your immune system considerably.
A lab study conducted in 2017 showed that a particular strain of probiotics, Bacillus bacteria, demonstrated anti-influenza activity, with complete inhibition of the influenza virus.
A 2017 systematic review and meta-analysis of randomized controlled trials evaluated the effects of probiotics and prebiotics on the immune response to the influenza vaccination. The results showed that participants who took probiotics and prebiotics showed significant improvements in the H1N1 and H3N2 strain protection rates. This suggests that taking probiotics may elevate your immunity.
11. Get Fresh Air
Indoor winter environments can be a source of concentrated toxins and germs. The dry air we inhale as we heat our homes during the winter makes airways more reactive and sensitive to viruses.
An added bonus to time spent outdoors in the winter is the extra bit of sunlight you receive.
12. Top Foods for Flu Recovery
Also, these are the best foods to consume while you recover from the flu.
Light, easy-to-digest foods: Include soups with bone broth, cooked vegetables, or herbal teas to help with digestion. Don’t force yourself to eat.
Water: Adequate hydration is the key to flushing out the virus from your system. Fluid helps your body to flush bacteria and viruses from your system. Drink approximately half your body weight in ounces daily of either spring water or reverse osmosis-filtered water. Green and black teas are potent immune system boosters and antioxidants. Try to drink at least eight ounces every two hours.
Hot water with lemon, honey, and cinnamon: Honey and cinnamon help prevent mucus buildup and keep you hydrated.
Ginger: Make ginger tea and add raw honey.
Garlic and onions: Both of these help boost immune function.
Personal Note:
Please I am not trying to scare anyone. My site is about awareness, and what you can do to safeguard yourselves. If you have the time please read my post:
10 Ten Threats to Global Health in 2019.
Always Visit Your Doctor and be Safe.
Thank you for reading,
Michael
Comments are welcome
Obviously you hear about getting your flu shot every year, I was unaware that it changed every year though to combat that years influenza strains. Unfortunately I work in a restaurant, so I am surrounded by people all day long. I have been fortunate in the part, but washing my hands constantly is a must, and trying to steer clear of people I notice coughing and sneezing a lot. Thank you for this useful information, I will be sure to pass it along to my friends and coworkers!
Hi Travis,
Thank you for your comments. I am glad to hear your taking the necessary precautions by washing your hands. Being in the restaurant business you have to be careful. Most of these diseases are airborne, and some people do not have the respect to cover their mouth when coughing, or sneezing, even washing their hands. Be safe.
Best wishes,
Michael
While reading the news, I was able to learn alot about the outbreak of the influenza flu. I used to call it a virus though. I see that there are a whole lot of people who are really dieing due to the flu. It is actually better to learn about it and how to prevent it than to get scared of the consequences. Your article has so much information on the topic and I should share with people so that they too can be aware. Nice one!
Hi henderson,
Thank you for your comments. The human immune system is suffering the strain of certain enviromental factors. Prevention and awarness are always important. What I write is not meant to scare anyone but make them aware, sharing the information may help someone.
Best wishes,
Michael
Hi,
I never knew the number of deaths from influenza was this high, or perhaps it is low to what it could be.
I do not think that I have ever had a vaccine for this but I know that a lot of elderly get this vaccine as well as children.
So far I have made it fine, I think I have gotten sick once or twice in a span of 10 years but with that being said when I get sick I usually need to go to the doctors and I have been in the risk factor with medications causing my immune system to get weakened.
I do think that it is good that you offer some statistics on the subject of influenza, because I have, for once, never realised that it can actually kill you if you are unfortunate enough to not be strong enough.
It is so important to have your children vaccinated. Not just to protect themselves but to also protect other children as you might till carry it without getting it.
Hi Alexandra,
Thank you for your comments. I did a blog on the 10 health scars that are facing us in the near future. Not to scare anyone, but just for everyone’s awareness, Influenza is listed to reach pandemic proporations. One of the many reasons I wanted to share this information. You mention your immune system getting weaker and this is something that is happening with many people. In many cases antibiotics are not as effective as they once used to be. If nothing else we have to take precautions for our children and elderly.
Best wishes,
Michael
What an interesting article and right on point. It really drives me nuts when that small percentage of our population actually believes that flu shots are bad for us. They can take that risk for themselves but when they also don’t take their children to get flu shots and then put them into the virus breeding-grounds that are schools and day-cares, its almost a certainty that some kind of bug will be picked up. I do hope that your article will help to reduce the uneducated in this area. I just got my flu shot last week.
Hi Feochadan,
Thank you for your comments. You are so right, prevention like taking that flu shot is so much better than the cure, or even worse the spread of disease. Children and the elderly are are at the greatest risk. I am glad you got your flu shot, as did I.
Best wishes,
Michael
Hello Michael, we all know this would scare anyone regardless of how hardened one’s heart can be. I have read about a worldwide epidemic breaking out much later in the future due to human activities with chemical and all, so i am curious to know, are you talking about something here?
Hi Benson,
Thank you for your comments. In one of my blogs I have mentioned the 10 scary health issues that are going to be affecting us. Influenza is supposed to reach pandemic proportions. It is so important we take the necessary precautions now. You are so right about the chemicals in the air affecting our health. Prevention is always better than the cure.
Best wishes,
Michael
There was no sign from the beginning of this post that I should not be scared about what I am about to read so to be honest, I was very scared about it. I must say that influenza is a very big killer. I just heard about it on the news and this discoveries are really shocking. I am happy that there are ways of preventing it though. Nice work that you put in here. Because you have pointed out that you want to do awareness with this, I will share this to help people also learn about this.
Hi John,
Thank you for your comments. It is scary as it is considered one of 10 major health issues that we may be facing. I appreciate you sharing your knowledge about influenza to the people you know. Prevention and awareness are very important.
Best wishes,
Michael
It really is one of the happiest things I have read today. The winter is slowly coming to Greece and the flu will be as threatening as last year’s health and lives of many people. It is vaccination that will save the lives of people vulnerable to human diseases. Prevention is the best cure. Your article is very enlightening and extremely informative.
Hi,
Thank you for your comments. You are so right, prevention is the best cure. It is getting cold here in Ontario, Canada also and I often hear about reminders to get a flu shot.
Best wishes,
Michael
Hi Michael, thank you for your article about influenza.Every time of the year ,influenza shows his face.we need to get prepared to fight.On the street and public transport,people are sneezing,coughing… It’s there you cannot escape.My concern is why do I catch influenza even though I did the vaccine?Do you know any natural remedy to fight it? Thank you!
Hi Eva,
Thank you for your comments.
Vaccines unfortunately are not a 100% precaution against any type of disease. Being aware of your surroundings is as important as washing your hands. If you are catching influenza on some kind of regular interval, seeing a Doctor is vital. Our immune systems are getting used to antibiotics, and even some vaccines. As always, nutrition, exercise, sleep and even sunliight are the best ways to avoid illness.
Best wishes,
Michael