What is meningitis?
Blue indicates link
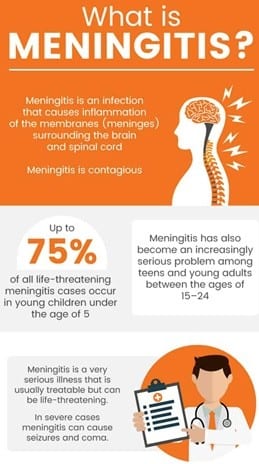
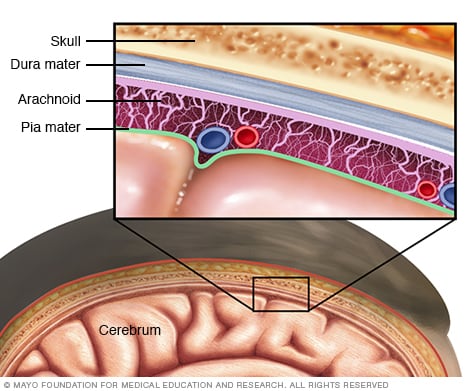
Meningitis is an acute inflammation of the protective membranes covering the brain and spinal cord, known collectively as the meninges. The most common symptoms are fever, headache, and neck stiffness. Other symptoms include confusion or altered consciousness, vomiting, and an inability to tolerate light or loud noises. Young children often exhibit only nonspecific symptoms, such as irritability, drowsiness, or poor feeding. If a rash is present, it may indicate a particular cause of meningitis; for instance, meningitis caused by meningococcal bacteria may be accompanied by a characteristic rash.
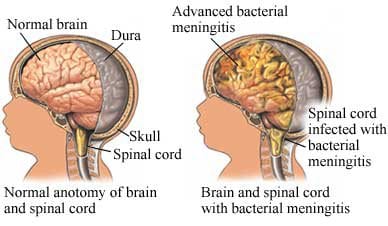
The inflammation may be caused by infection with viruses, bacteria, or other microorganisms, and less commonly by certain drugs. Meningitis can be life-threatening because of the inflammation’s proximity to the brain and spinal cord; therefore, the condition is classified as a medical emergency. A lumbar puncture, in which a needle is inserted into the spinal canal to collect a sample of cerebrospinal fluid (CSF), can diagnose or exclude meningitis.
Some forms of meningitis are preventable by immunization with the meningococcal, mumps, pneumococcal, and Hib vaccines. Giving antibiotics to people with significant exposure to certain types of meningitis may also be useful. The first treatment in acute meningitis consists of promptly giving antibiotics and sometimes antiviral drugs. Corticosteroids can also be used to prevent complications from excessive inflammation. Meningitis can lead to serious long-term consequences such as deafness, epilepsy, hydrocephalus, or cognitive deficits, especially if not treated quickly.
In 2015, meningitis occurred in about 8.7 million people worldwide. This resulted in 379,000 deaths—down from 464,000 deaths in 1990. With appropriate treatment, the risk of death in bacterial meningitis is less than 15%. Outbreaks of bacterial meningitis occur between December and June each year in an area of sub-Saharan Africa known as the meningitis belt. Smaller outbreaks may also occur in other areas of the world. The word meningitis comes from the Greek μῆνιγξ meninx, “membrane”, and the medical suffix -itis, “inflammation”.
Also, See:
Meningitis is an inflammation of the membranes (meninges) surrounding your brain and spinal cord. The swelling from meningitis typically triggers symptoms such as headache, fever, and a stiff neck.
Most cases of meningitis in the United States are caused by a viral infection, but bacterial, parasitic, and fungal infections are other causes. Some cases of meningitis improve without treatment in a few weeks. Others can be life-threatening and require emergency antibiotic treatment.
Seek immediate medical care if you suspect that someone has meningitis. Early treatment of bacterial meningitis can prevent serious complications.
Symptoms:
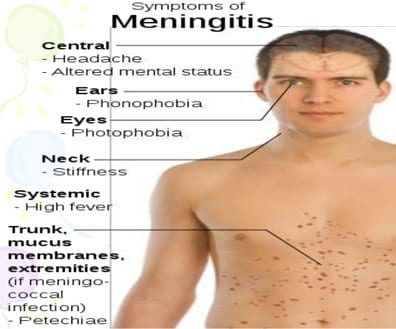
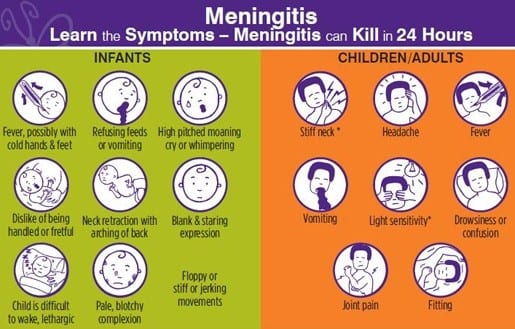
Early meningitis symptoms may mimic the flu (influenza). Symptoms may develop over several hours or over a few days.
Possible signs and symptoms in anyone older than the age of 2 include:
- Sudden high fever
- Stiff neck
- Severe headache that seems different than normal
- Headache with nausea or vomiting
- Confusion or difficulty concentrating
- Seizures
- Sleepiness or difficulty waking
- Sensitivity to light
- No appetite or thirst
- Skin rash (sometimes, such as in meningococcal meningitis)
Causes:
MeningitisOpen pop-up dialog box
Viral infections are the most common cause of meningitis, followed by bacterial infections and, rarely, fungal infections. Because bacterial infections can be life-threatening, identifying the cause is essential.
Bacterial meningitis:
Bacteria that enter the bloodstream and travel to the brain and spinal cord cause acute bacterial meningitis. But it can also occur when bacteria directly invade the meninges. This may be caused by an ear or sinus infection, a skull fracture, or, rarely, after some surgeries.
Several strains of bacteria can cause acute bacterial meningitis, most commonly:
- Streptococcus pneumoniae (pneumococcus). This bacterium is the most common cause of bacterial meningitis in infants, young children, and adults in the United States. It more commonly causes pneumonia or ear or sinus infections. A vaccine can help prevent this infection.
- Neisseria meningitidis (meningococcus). This bacterium is another leading cause of bacterial meningitis. These bacteria commonly cause an upper respiratory infection but can cause meningococcal meningitis when they enter the bloodstream. This is a highly contagious infection that affects mainly teenagers and young adults. It may cause local epidemics in college dormitories, boarding schools, and military bases. A vaccine can help prevent infection.
- Haemophilus influenzae (Haemophilus). Haemophilus influenzae type b (Hib) bacterium was once the leading cause of bacterial meningitis in children. However, new Hib vaccines have greatly reduced the number of cases of this type of meningitis.
- Listeria monocytogenes (listeria). These bacteria can be found in unpasteurized cheeses, hot dogs, and lunch meats. Pregnant women, newborns, older adults, and people with weakened immune systems are most susceptible. Listeria can cross the placental barrier, and infections in late pregnancy may be fatal to the baby.
Viral meningitis:
Viral meningitis is usually mild and often clears on its own. Most cases in the United States are caused by a group of viruses known as enteroviruses, which are most common in late summer and early fall. Viruses such as herpes simplex virus, HIV, mumps, West Nile virus, and others also can cause viral meningitis.
Chronic meningitis:
Slow-growing organisms (such as fungi and Mycobacterium tuberculosis) that invade the membranes and fluid surrounding your brain cause chronic meningitis. Chronic meningitis develops over two weeks or more. The signs and symptoms of chronic meningitis — headaches, fever, vomiting, and mental cloudiness — are similar to those of acute meningitis.
Fungal meningitis:
Fungal meningitis is relatively uncommon and causes chronic meningitis. It may mimic acute bacterial meningitis. Fungal meningitis isn’t contagious from person to person. Cryptococcal meningitis is a common fungal form of the disease that affects people with immune deficiencies, such as AIDS. It’s life-threatening if not treated with an anti-fungal medication.
Other meningitis causes:
Meningitis can also result from noninfectious causes, such as chemical reactions, drug allergies, some types of cancer, and inflammatory diseases such as sarcoidosis.
Risk factors:
Risk factors for meningitis include:
- Skipping vaccinations. Risk rises for anyone who hasn’t completed the recommended childhood or adult vaccination schedule.
- Age. Most cases of viral meningitis occur in children younger than age 5. Bacterial meningitis is common in those under the age of 20.
- Living in a community setting. College students living in dormitories, personnel on military bases, and children in boarding schools and childcare facilities are at greater risk of meningococcal meningitis. This is probably because the bacterium is spread by the respiratory route, and spreads quickly through large groups.
- Pregnancy. Pregnancy increases the risk of listeriosis — an infection caused by listeria bacteria, which may also cause meningitis. Listeriosis increases the risk of miscarriage, stillbirth, and premature delivery.
- Compromised immune system. AIDS, alcoholism, diabetes, the use of immunosuppressant drugs, and other factors that affect your immune system also make you more susceptible to meningitis. Having your spleen removed also increases your risk, and anyone without a spleen should get vaccinated to minimize that risk.
Complications:
Meningitis complications can be severe. The longer you or your child has the disease without treatment, the greater the risk of seizures and permanent neurological damage, including:
- Hearing loss
- Memory difficulty
- Learning disabilities
- Brain damage
- Gait problems
- Seizures
- Kidney failure
- Shock
- Death
With prompt treatment, even patients with severe meningitis can recover.
Prevention:
Common bacteria or viruses that can cause meningitis can spread through coughing, sneezing, kissing, or sharing eating utensils, a toothbrush, or a cigarette.
These steps can help prevent meningitis:
- Wash your hands. Careful hand-washing helps prevent the spread of germs. Teach children to wash their hands often, especially before eating and after using the toilet, spending time in a crowded public place, or petting animals. Show them how to vigorously, and thoroughly wash and rinse their hands.
- Practice good hygiene. Don’t share drinks, foods, straws, eating utensils, lip balms, or toothbrushes with anyone else. Teach children and teens to avoid sharing these items too.
- Stay healthy. Maintain your immune system by getting enough rest, exercising regularly, and eating a healthy diet with plenty of fresh fruits, vegetables, and whole grains.
- Cover your mouth. When you need to cough or sneeze, be sure to cover your mouth and nose.
- If you’re pregnant, take care of the food you eat. Reduce your risk of listeriosis by cooking meat, including hot dogs and deli meat, to 165 F (74 C). Avoid cheeses made from unpasteurized milk. Choose cheeses that are clearly labeled as being made with pasteurized milk.
Immunizations:
Some forms of bacterial meningitis are preventable with the following vaccinations:
- Haemophilus influenzae type b (Hib) vaccine. Children in the United States routinely receive this vaccine as part of the recommended schedule of vaccines, starting at about 2 months of age. The vaccine is also recommended for some adults, including those who have sickle cell disease or AIDS and those who don’t have a spleen.
- Pneumococcal conjugate vaccine (PCV13). This vaccine also is part of the regular immunization schedule for children younger than 2 years in the United States. Additional doses are recommended for children between the ages of 2 and 5 who are at high risk of pneumococcal disease, including children who have chronic heart or lung disease or cancer.
- Pneumococcal polysaccharide vaccine (PPSV23). Older children and adults who need protection from pneumococcal bacteria may receive this vaccine. The Centers for Disease Control and Prevention recommends the PPSV23 vaccine for all adults older than 65; for younger adults and children age 2 and older who have weak immune systems or chronic illnesses such as heart disease, diabetes, or sickle cell anemia; and for anyone who doesn’t have a spleen.
- Meningococcal conjugate vaccine. The Centers for Disease Control and Prevention recommends that a single dose be given to children ages 11 to 12, with a booster shot given at age 16. If the vaccine is first given between ages 13 and 15, the booster is recommended between ages 16 and 18. If the first shot is given at age 16 or older, no booster is necessary. This vaccine can also be given to children between the ages of 2 months and 10 years who are at high risk of bacterial meningitis or who have been exposed to someone with the disease. It’s also used to vaccinate healthy but previously unvaccinated people who have been exposed through outbreaks.
How is meningitis treated?
Your treatment is determined by the cause of your meningitis.
Bacterial meningitis requires immediate hospitalization. Early diagnosis and treatment will prevent brain damage and death. Bacterial meningitis is treated with intravenous antibiotics. There’s no specific antibiotic for bacterial meningitis. It depends on the bacteria involved.
Fungal meningitis is treated with anti-fungal agents.
Parasitic meningitis may either involve treating just the symptoms or attempting to treat the infection directly. Depending on the cause, this type may get better without antibiotic treatment. If it worsens, however, your doctor may try to treat the infection itself.
Viral meningitis may resolve on its own, but some causes of viral meningitis will be treated with intravenous antiviral medications.
How contagious is meningitis?
Several types of meningitis are not contagious. Fungal, parasitic, and non-infectious meningitis is not contagious.
Viral meningitis is contagious. It’s spread through direct contact with body fluids, including mucus, feces, and saliva. Droplets of infected fluid can be spread and shared with sneezing and coughing. You do not have to come into direct contact with an infected person to pick up this infection.
Bacterial meningitis, the most serious form of meningitis, can also be contagious, especially if it’s meningococcal meningitis. It’s spread through extended contact with an infected person. Schools, daycare centers, military barracks, hospitals, and college dormitories are prime locations for sharing this infection. Some types of meningitis are spread through person-to-person contact but not all.
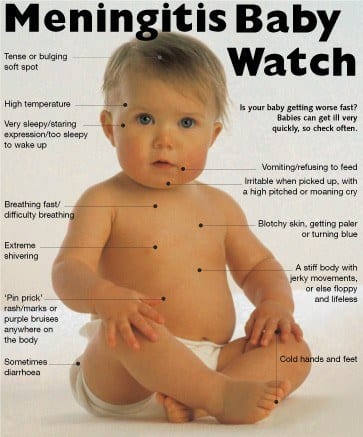
Meningitis in an infant:
Babies who develop meningitis may show different signs and symptoms of infection than adults. These symptoms can include:
- fever
- jaundice
- body or neck stiffness
- high-pitched crying
- inconsolable behaviors
- sleepy and difficulty waking
- irritable and grumpy
- doesn’t feel well and has a weak suck during breastfeeding
Viral meningitis is common in infants. It develops as a result of colds, cold sores, flu, and diarrhea. The viruses that cause these common conditions also cause viral meningitis.
Bacterial meningitis, which is common but life-threatening, most likely spreads from a serious infection in a nearby area of the body. For example, bacteria from a severe ear infection or sinus infection can enter the bloodstream and find their way to the brain or spinal cord and cause a bigger infection.
Meningitis in children:
Meningitis becomes more common in children as they grow older and reach high school and college ages. Symptoms of viral and bacterial meningitis in children are very similar to symptoms in adults. These include:
- sudden fever
- body and neck aches
- confusion or disorientation
- nausea
- vomiting
- tiredness or fatigue
Meningitis in adults:
The risk for several forms of meningitis decreases after young adulthood. That’s in large part due to changing circumstances. Schools and college dormitories are common sites where some forms of meningitis can be easily shared. Once a young adult ages out of these settings, the likelihood of infection begins to fall.
However, after age 60, the risk starts to rise again. That’s because of underlying diseases or health conditions that weaken the immune systems in older individuals.
Adults with a compromised immune system are at a greater risk of developing meningitis. Likewise, adults in environments where individuals are in close contact with one another may be at greater risk for an infection. This includes teachers, healthcare providers, and daycare staffers.
How is meningitis diagnosed?
Diagnosing meningitis starts with a health history and physical exam. Age, dorm residence, and daycare center attendance can be important clues. During the physical exam, your doctor will look for:
- a fever
- an increased heart rate
- neck stiffness
- reduced consciousness
Your doctor will also order a lumbar puncture. This test is also called a spinal tap. It allows your doctor to look for increased pressure in the central nervous system. It can also find inflammation or bacteria in the spinal fluid. This test can also determine the best antibiotic for treatment.
Other tests may also be ordered to diagnose meningitis. Common tests include the following:
- Blood cultures identify bacteria in the blood. Bacteria can travel from the blood to the brain. N. meningitidis and S. Pneumonia, among others, can cause both sepsis and meningitis.
- A complete blood count with differential is a general index of health. It checks the number of red and white blood cells in your blood. White blood cells fight infection. The count is usually elevated in meningitis.
- Chest X-rays can reveal the presence of pneumonia, tuberculosis, or fungal infections. Meningitis can occur after pneumonia.
- A CT scan of the head may show problems like a brain abscess or sinusitis. Bacteria can spread from the sinuses to the meninges.
Your doctor may also conduct a glass test. For this test, your doctor will roll a glass over the meningitis rash. If the rash doesn’t fade under the pressure, it’s likely a meningitis rash. If it does fade, the unusual spots on the skin may be the result of another condition. How is meningitis prevented?
Maintaining a healthy lifestyle, especially if you’re at increased risk, is important. This includes:
- getting adequate amounts of rest
- not smoking
- avoiding contact with sick people
If you’ve been in close contact with one or more people who have a bacterial meningococcal infection, your doctor can give you preventive antibiotics. This will decrease your chances of developing the disease.
Vaccinations can also protect against certain types of meningitis. Vaccines that can prevent meningitis include the following:
- Haemophilus influenzae type B (Hib) vaccine
- pneumococcal conjugate vaccine
- meningococcal vaccine
Practicing good personal hygiene may also help you prevent meningitis. Some types of meningitis are spread through close contact with an infected person’s body fluid, such as saliva and nasal secretions. Avoid sharing drinks, utensils, and personal items that may carry saliva or other fluids.
What are the complications of meningitis?
These complications are typically associated with meningitis:
- seizures
- hearing loss
- vision loss
- memory problems
- arthritis
- migraine headaches
- brain damage
- hydrocephalus
- a subdural empyema, or a buildup of fluid between the brain and the skull
A meningitis infection may produce bacteria in the bloodstream. These bacteria multiply and some release toxins. That can cause blood vessel damage and leaking of blood into the skin and organs.
A serious form of this blood infection can be life-threatening. Gangrene may damage skin and tissue. In rare cases, amputation may be necessary. Several other serious complications may occur in people with meningitis.
Meningitis and pneumonia:
Pneumococcal meningitis is a rare but serious and life-threatening form of bacterial meningitis. Even with treatment, 20 percent of people with this type of infection die.
About 40 percent of people carry bacteria called Streptococcus pneumoniae in their throat and the back of the nose. These bacteria are responsible for common illnesses like pneumonia, sinus infections, and ear infections.
From time to time, however, those bacteria manage to cross the blood-brain barrier and cause inflammation and infection in the brain, spinal cord, or fluids immediately surrounding them.
Symptoms of this serious form of meningitis include:
- chills
- high fever
- vomiting
- chest pain
- headache
- cough
- confusion
- weakness
- disorientation
Fortunately, two vaccines are available to prevent pneumococcal meningitis. What are the risk factors for meningitis?
The following are some of the risk factors for meningitis:
Compromised immunity:
People with immune deficiency are more vulnerable to infections. This includes the infections that cause meningitis. Certain disorders and treatments can weaken your immune system. These include:
- HIV/AIDS
- autoimmune disorders
- chemotherapy
- organ or bone marrow transplants
Cryptococcal meningitis, which is caused by a fungus, is the most common form of meningitis in people with HIV.
Community living:
Meningitis is easily spread when people live in close quarters. Being in small spaces increases the chance of exposure. Examples of these locations include:
- college dormitories
- barracks
- boarding schools
- daycare centers
Pregnancy:
Pregnant women have an increased risk of listeriosis, which is an infection caused by Listeria bacteria. Infection can spread to the unborn child.
Age:
All ages are at risk for meningitis. However, certain age groups have a higher risk. Children under the age of 5 are at increased risk of viral meningitis. Infants are at higher risk of bacterial meningitis.
Working with animals:
Farmworkers and others who work with animals have an increased risk of infection with Listeria.
Related stories:
 Infographic: What Your Teen Needs to Bring to College or Camp to Prevent Meningitis
Infographic: What Your Teen Needs to Bring to College or Camp to Prevent Meningitis Talking to Your Teen About Meningitis
Talking to Your Teen About Meningitis Aseptic Meningitis
Aseptic Meningitis How Can I Avoid Getting Meningitis?
How Can I Avoid Getting Meningitis? How to Recognize Kernig’s Sign
How to Recognize Kernig’s Sign
Are There Herbal Remedies for Meningitis?
ALWAYS CONSULT WITH YOUR DOCTOR FIRST. THERE ARE DIFFERENT TYPES OF MENINGITIS.
Garlic
Garlic can be very beneficial for those suffering from meningitis as the allicin and various other organic compounds act as powerful antioxidants that have antiviral and antibacterial properties.
Olive Leaf Extract
For an herbal approach to relief from meningitis, you can turn to olive leaf extract, which has antiviral and antioxidant properties, in addition to its proven anti-inflammatory abilities.
Chlorella
One of the most well-known home remedies for meningitis is chlorella, a small plant that packs a major punch, due to its impressive chlorophyll content. Chlorophyll is remarkably similar in structure to hemoglobin, so, it can boost red blood cell production, which increases oxygenation, purifies the blood, and helps speed up recovery and repair of the damage from meningitis.
Bed Rest
Although this seems like an obvious suggestion, the compromised immune system caused by meningitis means that any further (and unnecessary) exposure to pathogens or viruses can make the entire situation even more complicated. Therefore, a patient should get comfortable, stock up on books and movies, and stay in bed until their body can naturally heal.
Cold Packs
The fever that accompanies meningitis can often be quite severe, and it can also make treatment and recovery more difficult. Fevers are a red flag that your body is fighting off an infection, but the raised temperature can be dangerous in and of itself. Regularly using ice packs to keep the fever down can give your immune system more of a fighting chance against inflammation and infection.
Neutral Bath
When you slide into a neutral temperature bath, your blood will respond accordingly and redistribute properly throughout your body, thereby easing the inflammation and discomfort in the brain and spinal cord, effectively treating some of the symptoms.
Ginseng
The active ingredients of ginseng called ginsenosides are believed to directly act on the affected membranes to eliminate the infection and speed the recovery process of meningitis. Ginseng can be eaten directly or boiled in tea to enjoy the benefits of this ancient remedy in getting you to bounce back
Reishi Mushrooms
The triterpenes and polysaccharides found in reishi mushrooms promote a stronger immune system and can help reduce the dangerous inflammation caused by meningitis.
Astragalus
With a host of saponins and flavonoids, this herb is able to rapidly bring the immune system back to normal and clear up many of the most uncomfortable symptoms of meningitis. Astragalus is considered one of the most effective home remedies for this terrible condition.
Drink Water:
Hydration is key when it comes to naturally overcoming meningitis. Drinking water helps to flush excess waste, including bacteria and proteins, from the body and keeps them from building up in your kidneys. It is recommended to drink half your body weight in ounces of water to stay sufficiently hydrated. If you weigh 150 pounds and divide that by two to get 75, you should drink 75 ounces every day. You may need to drink more when you have meningitis. Try to avoid juice because it contains a lot of sugar and can worsen inflammation.
Soybean milk:
This plays an important role in meningitis by strengthening the immune system and speeding up the process of healing; you can mix soybean milk with honey and take this drink before going to bed. This is a natural meningitis cure and it can be used for three to four months.
Coconut oil:
This wonderful oil can eliminate meningitis, even the type caused by fungi; it inhibits the growth of fungi or yeast and can be used as an alternative anti-fungal treatment.
The healthy fatty acids present in this oil help the body to absorb nutrients, and increase the body’s metabolism and it is stored as energy in the body; apart from fungi, it also has antibacterial, antiviral, and antimicrobial properties making the oil an all-round health booster.
Cat’s claw
This ancient herb is used to cure meningitis; it has good anti-inflammatory compounds that cure meningitis effectively, it also boosts the immune system and hastens the healing process.
Goldenseal
The root of this ancient herb has powerful medicinal properties and it is potent against meningitis; it is loaded with antibacterial and anti-fungal compounds that can be used to cure this condition.
You can take herbal tea consisting of goldenseal and Echinacea to boost your immune system and hasten your healing.
Hypericum
This powerful herb contains an active compound called hyperforin; this wonderful herb has antiviral and antibacterial properties and it can cut through the blood-brain barrier. This herb is potent against bacteria that cause meningitis.
Home Precautions:
Avoid the intake of liquid-based foods
Aside from the usual medical treatment prescribed by doctors, an assistive management procedure is to avoid the intake of liquid foods. This is especially important during the first few days of treatment. The only liquid that can be provided to a patient is oral rehydration salt combined with lukewarm water for regular consumption.
Patients may also be provided with fruit juice after a few days. Fruit juices feature high nutritional content that boosts body resistance as well as energy. Increased fluid intake also increases urinary output which adds to relief from unwanted symptoms.
How about Vitamins and Minerals?
All I could find was:
Ginseng
Vitamin C
Word of Caution: The bacterial form of meningitis is more dangerous than the viral form, but both should be treated quite seriously. The above recommendations are viable options in conjunction with formal medical treatment. In particular, if the diagnosis/treatment is delayed for some reason, more aggressive treatment will be necessary to ensure that no permanent damage is done.
Please if you have any symptoms of meningitis, it is highly recommended you seek medical help.
Thank you for reading,
Michael.
Comments are welcome





Hello Michael – Many thanks for this completely thorough article on meningitis I have heard of this infection but not to this degree. I didn’t realize that there were so many variations. We certainly live in an infectious environment more so now than ever. We must be vigilant in fending off these infections by following the rules. The most basic of these are: wash the hands!
Thanks for this opportunity!
Hi Nathaniel,
Thank you for your comments. I am trying to cover the diseases that fall under the coronaviruses umbrella. We certainly have to build up our immune systems. It is almost like history is repeating itself.
Best wishes and stay healthy,
Michael