What is the pancreas?
Blue indicates link
The pancreas is a glandular organ in the digestive system and endocrine system located in the abdominal cavity behind the stomach. It is an endocrine gland producing several important hormones, including insulin, glucagon, somatostatin, and pancreatic polypeptide, all of which circulate in the blood.
The pancreas is an abdominal organ that is located behind the stomach and is surrounded by other organs, including the spleen, liver, and small intestine. The pancreas is about 6 inches (15.24 centimeters) long, oblong, and flat.
The pancreas plays an important role in digestion and in regulating blood sugar. Three diseases associated with the pancreas are pancreatitis, pancreatic cancer, and diabetes.
Location of the pancreas:
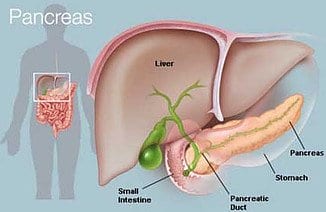
The pancreas is located in the upper abdomen behind the stomach,” Knowlton said. The right end of the pancreas is wide and called the head. From the head, the organ tapers to the left. The middle sections are called the neck and body, while the narrow end on the left side of the body is called the tail.
The function of the pancreas:
The pancreas serves two primary functions, according to Jordan Knowlton, an advanced registered nurse practitioner at the University of Florida Health Shands Hospital. It makes “enzymes to digest proteins, fats, and carbs in the intestines” and produces the hormones insulin and glucagon.
Insulin also allows glucose to enter muscle and other tissue, works with the liver to store glucose and synthesize fatty acids, and “stimulates the uptake of amino acids,” according to Bowen. Insulin is released after eating protein and especially after eating carbohydrates, which increase glucose levels in the blood. If the pancreas does not produce sufficient insulin, type 1 diabetes will develop.
Unlike insulin, glucagon raises blood sugar levels. According to the Johns Hopkins University Sol Goldman Pancreatic Cancer Research Center, the combination of insulin and glucagon maintains the proper level of sugar in the blood.
The pancreas’ second, exocrine function is to produce and release digestive fluids. After food enters the stomach, digestive enzymes called pancreatic juice travel through several small ducts to the main pancreatic duct and then to the bile duct, according to the Medical University of South Carolina’s Digestive Disease Center. The bile duct takes the juice to the gallbladder, where it mixes with bile to aid in digestion.
Pancreas pain:
Intense pancreatic pain is usually associated with acute pancreatitis. It can be hard to identify pancreas pain and evaluate pancreas diseases because the organ sits deep in the abdomen, according to The National Pancreas Association. Other signs that the pain may be pancreatic include jaundice, itchy skin, and unexplained weight loss. If you are experiencing pancreas pain, consult your doctor.
Pancreatitis:

The National Institutes of Health defines pancreatitis as inflammation of the pancreas, happening when “digestive enzymes start digesting the pancreas itself.” It can be acute or chronic, but both forms should be taken seriously and may lead to additional health problems.
Chronic pancreatitis
There are up to 23 cases of chronic pancreatitis per 100,000 people per year worldwide. In the United States, it results in more than 122,000 outpatient visits and more than 56,000 hospitalizations per year, according to the Cleveland Clinic.
“Chronic pancreatitis is a persistent inflammation (greater than three weeks) of the pancreas that causes permanent damage,” Knowlton said. The condition is often caused by “heavy, ongoing” alcohol consumption, but she added that there are other causes, including “those that cause acute pancreatitis attacks.” Other causes may be cystic fibrosis, high levels of calcium or fat in the blood, and autoimmune disorders.
Symptoms include upper abdominal pain, nausea, vomiting, weight loss, and oily stools. According to Peter Lee and Tyler Stevens, in an article for the Cleveland Clinic, “clinically apparent” oily stools (steatorrhea) do not appear until “90 percent of pancreatic function has been lost.”
“Chronic pancreatitis requires dietary modifications, including a low-fat diet and cessation of alcohol [intake] and smoking,” Knowlton said. Chronic pancreatitis does not heal and tends to worsen with time, and “treatment options are mostly for pain relief.” She added that treatments “may include a pancreas stent or, for severe cases, surgery (either a lateral pancreaticojejunostomy or a Whipple procedure).” Pancreatiocojejunostomies are designed to decrease pancreatic leakage while the Whipple procedure removes the head of the pancreas where, according to the Mayo Clinic, most tumors occur.

There may be a link between chronic pancreatitis and pancreatic cancer. According to the University of California Los Angeles Center for Pancreatic Diseases, “Recent studies reveal a 2-5 times increase in the incidence of pancreatic cancer in patients with chronic pancreatitis from a variety of causes.”
Acute pancreatitis
“Acute pancreatitis is inflammation of the pancreas (lasting less than three weeks), that is most often caused by gallstones,” said Knowlton. It usually comes on suddenly and disappears within a few days of treatment. In addition to gallstones, Knowlton said that causes “may include medications, high triglycerides, high calcium in the blood, and high alcohol consumption.”
Pancreas pain is the chief symptom of acute pancreatitis, according to Medscape. The pain is usually severe and sudden. It increases in severity until it becomes a constant ache. This pancreas pain is felt in the upper abdomen. The Mayo Clinic noted that the pain can radiate through to the back, and Knowlton pointed out that it might be worse after eating. Other symptoms of acute pancreatitis include nausea, vomiting, fever, and diarrhea.
According to Knowlton, “This patient often looks acutely ill, and requires hospitalization (typically for three to five days), intravenous (IV) hydration, nothing by mouth (for bowel rest), pain medication, treatment of underlying conditions, and possibly a radiologic procedure called an endoscopic retrograde cholangiopancreatography (ERCP), which can more specifically target the problem.” If the acute pancreatitis was caused by gallstones, doctors may recommend removing the gallbladder.
Pancreatic cancer:
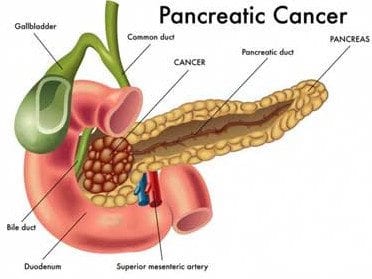
It is hard to diagnose pancreatic cancer early. The Mayo Clinic noted that symptoms typically don’t occur until the cancer has advanced. Knowlton said, “Unfortunately, symptoms can be vague, but can include abdominal pain, jaundice, severe itching, weight loss, nausea, vomiting, and digestive problems.”
Making matters even more complicated is the pancreas’ deep-in-the-abdomen location. The NIH pointed out that as a result, tumors cannot usually be felt by touch. Because of the difficulty of early diagnosis and the rapidity with which pancreatic cancer spreads, the prognosis is often poor.
Risk factors for pancreatic cancer include smoking, long-term diabetes, and chronic pancreatitis, according to the National Cancer Institute.
According to the American Cancer Society, pancreatic cancer usually begins in the cells that produce pancreatic (digestive) juices or in the cells that line the ducts. On rare occasions, pancreatic cancer will begin in the cells that produce hormones.
According to the University of Texas MD Anderson Cancer Center, to diagnose pancreatic cancer, doctors typically conduct physical exams, blood tests, imaging tests, endoscopic ultrasounds and tests, and biopsies. Treatment options include surgery, radiation, chemotherapy, and therapies targeted to attack cancer cells without harming normal cells.
Pancreatic cancer begins in the tissues of your pancreas — an organ in your abdomen that lies behind the lower part of your stomach. Your pancreas releases enzymes that aid digestion and produce hormones that help manage your blood sugar.
Several types of growths can occur in the pancreas, including cancerous and noncancerous tumors. The most common type of cancer that forms in the pancreas begins in the cells that line the ducts that carry digestive enzymes out of the pancreas (pancreatic ductal adenocarcinoma).
Pancreatic cancer is seldom detected at its early stages when it’s most curable. This is because it often doesn’t cause symptoms until after it has spread to other organs.
Pancreatic cancer treatment options are chosen based on the extent of the cancer. Options may include surgery, chemotherapy, radiation therapy, or a combination of these.
More on Pancreas problems:
- It is important to be aware of what is going on with your health and when experiencing symptoms of pancreas problems careful attention is necessary to understand and investigate the problem
- Many of the symptoms are the same whether you experience an inflamed pancreas or pancreas tumor
- Most people get alarmed when they experience pain in the abdomen associated with symptoms of pancreas problems and automatically think it is cancer, however, cancer of the pancreas can bring about its own set of symptoms
- The only sure sign of diagnosis is to have the pancreas enzymes examined and tested to accurately identify what your symptoms mean
Below is a list of 7 symptoms of pancreas problems related to an inflamed pancreas, pancreas tumor, and even cancer of the pancreas. This information is important and should not be overlooked when experiencing any of the following symptoms.
1. Yellow tint to skin and eyes
A yellow tint to your skin and eyes could indicate jaundice, especially if accompanied by skin itching. Jaundice can be related to gallstones, liver problems, hepatitis, and most commonly cancer. In the event that you experience jaundice associated with pancreas problems, it is necessary to have diagnostic testing done right away as cancer of the pancreas can spread into the lymph nodes quickly.
2. Loss of weight and appetite
This symptom is difficult to rule as to which pancreas problem you may be experiencing. An inflamed pancreas can cause you not to want to eat anything but liquid foods such as broth or gelatin, in which case you are bound to lose weight. Cancer of the pancreas can also cause significant weight loss and it is best to be seen by a healthcare professional so that your pancreas enzymes can be examined.
3. Nausea and vomiting
One of the more common symptoms of pancreas problems is nausea and vomiting. When a person has a pancreas tumor this can cause a loss of appetite and nausea. Also, the person may vomit when they eat depending on the location of the tumor. An inflamed pancreas can also cause an upset stomach. If symptoms persist it is wise to have testing done by your physician.
4. Diarrhea
Diarrhea could be a sign that your pancreas enzymes are insufficient. Insufficiency can cause diarrhea. Weight loss is usually accompanied by diarrhea and is one of the more common symptoms of pancreas problems. If the diarrhea is prolonged you should visit your health care professional to alleviate dehydration.
5. Dull pain in the upper abdomen
Dull pain in the upper abdomen can be a result of pancreatic cancer. Cancer of the pancreas results in abdominal pain accompanied by yellow skin tints or jaundice.
6. Mood changes and depression
As with any pancreas problems, the pain or overall symptoms can cause your mood to change and depression to set in. If you are feeling overwhelmed it is important to inform your doctor so that he or she can provide the support you need.
7. Fatigue
As with any symptoms of pancreas problems, fatigue can occur because your body is working overtime to heal itself. Ample rest is required but should not be ignored. If you do not feel like yourself and fatigue is taking over, it is important to see your physician right away.
Reasons for Problems with your Pancreas:
Acute pancreatitis causes include:
- Autoimmune diseases
- Drinking lots of alcohol
- Infections
- Gallstones
- Medications
- Metabolic disorders
- Surgery
- Trauma
In up to 15% of people with acute pancreatitis, the cause is unknown.
Chronic pancreatitis causes include:
- Cystic fibrosis
- Family history of pancreas disorders
- Gallstones
- High triglycerides
- Longtime alcohol use
- Medications
In about 20% to 30% of cases, the cause of chronic pancreatitis is unknown. People with chronic pancreatitis are usually men between the ages of 30 and 40.
More conditions that can lead to pancreatitis include:
- Abdominal surgery
- Alcoholism
- Certain medications
- Cystic fibrosis
- Gallstones
- High calcium levels in the blood (hypercalcemia), which may be caused by an overactive parathyroid gland (hyperparathyroidism)
- High triglyceride levels in the blood (hypertriglyceridemia)
- Infection
- Injury to the abdomen
- Obesity
- Pancreatic cancer
Risk factors:
Factors that increase your risk of pancreatitis include:
- Excessive alcohol consumption. Research shows that heavy alcohol users (people who consume four to five drinks a day) are at increased risk of pancreatitis.
- Cigarette smoking. Smokers are on average three times more likely to develop chronic pancreatitis, compared with nonsmokers. The good news is quitting smoking decreases your risk by about half
- Obesity. You’re more likely to get pancreatitis if you’re obese.
- Family history of pancreatitis. The role of genetics is becoming increasingly recognized in chronic pancreatitis. If you have family members with the condition, your odds increase — especially when combined with other risk factors.
Pancreatitis can cause serious complications, including:
- Pseudocyst. Acute pancreatitis can cause fluid and debris to collect in cyst-like pockets in your pancreas. A large pseudocyst that ruptures can cause complications such as internal bleeding and infection.
- Infection. Acute pancreatitis can make your pancreas vulnerable to bacteria and infection. Pancreatic infections are serious and require intensive treatment, such as surgery to remove the infected tissue.
- Kidney failure. Acute pancreatitis may cause kidney failure, which can be treated with dialysis if kidney failure is severe and persistent.
- Breathing problems. Acute pancreatitis can cause chemical changes in your body that affect your lung function, causing the level of oxygen in your blood to fall to dangerously low levels.
- Diabetes. Damage to insulin-producing cells in your pancreas from chronic pancreatitis can lead to diabetes, a disease that affects the way your body uses blood sugar.
- Malnutrition. Both acute and chronic pancreatitis can cause your pancreas to produce fewer of the enzymes that are needed to break down and process nutrients from the food you eat. This can lead to malnutrition, diarrhea, and weight loss, even though you may be eating the same foods or the same amount of food.
- Pancreatic cancer. Long-standing inflammation in your pancreas caused by chronic pancreatitis is a risk factor for developing pancreatic cancer.
Treatment:
Initial treatments in the hospital may include:
- Fasting. You’ll stop eating for a couple of days in the hospital in order to give your pancreas a chance to recover. Once the inflammation in your pancreas is controlled, you may begin drinking clear liquids and eating bland foods. With time, you can go back to your normal diet. If your pancreatitis persists and you still experience pain when eating, your doctor may recommend a feeding tube to help you get nutrition.
- Pain medications. Pancreatitis can cause severe pain. Your healthcare team will give you medications to help control the pain.
- Intravenous (IV) fluids. As your body devotes energy and fluids to repairing your pancreas, you may become dehydrated. For this reason, you’ll receive extra fluids through a vein in your arm during your hospital stay.
Once your pancreatitis is under control, your healthcare team can treat the underlying cause of your pancreatitis. Depending on the cause of your pancreatitis, treatment may include:
-
- Procedures to remove bile duct obstructions. Pancreatitis caused by a narrowed or blocked bile duct may require procedures to open or widen the bile duct.
A procedure called endoscopic retrograde cholangiopancreatography (ERCP) uses a long tube with a camera on the end to examine your pancreas and bile ducts. The tube is passed down your throat, and the camera sends pictures of your digestive system to a monitor.
ERCP can aid in diagnosing problems in the bile duct and pancreatic duct and in making repairs. In some people, particularly the elderly, ERCP can also lead to acute pancreatitis.
- Gallbladder surgery. If gallstones cause your pancreatitis, your doctor may recommend surgery to remove your gallbladder (cholecystectomy).
- Pancreas surgery. Surgery may be necessary to drain fluid from your pancreas or to remove diseased tissue.
- Treatment for alcohol dependence. Drinking several drinks a day over many years can cause pancreatitis. If this is the cause of your pancreatitis, your doctor may recommend you enter a treatment program for alcohol addiction. Continuing to drink may worsen your pancreatitis and lead to serious complications.
Additional treatments for chronic pancreatitis:
Depending on your situation, chronic pancreatitis may require additional treatments, including:
- Pain management. Chronic pancreatitis can cause persistent abdominal pain. Your doctor may recommend medications to control your pain and may refer you to a pain specialist. Severe pain may be relieved with options such as endoscopic ultrasound or surgery to block nerves that send pain signals from the pancreas to the brain.
- Enzymes to improve digestion. Pancreatic enzyme supplements can help your body break down and process the nutrients in the foods you eat. Pancreatic enzymes are taken with each meal.
- Changes to your diet. Your doctor may refer you to a dietitian who can help you plan low-fat meals that are high in nutrients.
ALWAYS SEE YOUR DOCTOR FIRST
Alternative Home Remedies after consultation with your Physician
Blueberries
The presence of free radicals can aggravate or bring about pancreatitis. One of the best free-radical-fighting foods you can eat is blueberries, which are packed with antioxidants and can reduce inflammation throughout the body very rapidly. Eating a handful of blueberries every morning can lower your risk of suffering from this condition.
Tofu
Switching to tofu-based meals is a popular meat alternative for people, particularly those who suffer from chronic pancreatitis. This is because high levels of fat in the blood are one of the most common causes of pancreatitis, which can be caused by eating a lot of red meat. If you cut out high-fat foods, such as red meat, you can lower your chances of inflammation in the pancreas.
Ginseng
Ginseng is one of the oldest and most trusted natural remedies for a wide variety of health issues, especially those that are inflammatory in nature or affect the gastrointestinal system. For a case of pancreatitis, ginseng tea or ginseng root supplements can be taken to lower inflammation throughout the body and relieve pain.
Acupuncture
Acupuncture is an ancient remedy for pancreatitis, and there are a number of key pressure points and areas of the body where acupuncture can relieve the pain and inflammation of this particular gland in your body.
Yogurt
People consume yogurt for many reasons, but it is primarily to regulate the balance of bacteria in the stomach to improve digestive efficiency and prevent infections in the gut. This can significantly strengthen the immune system, which can then work harder to reduce inflammation in other areas and glands near the stomach, such as the pancreas.
Reishi Mushrooms
This particular variety of mushrooms is one of the most densely packed foods when it comes to antioxidants and active organic compounds that can affect our health. In pancreatitis, reishi mushrooms are able to soothe the stomach and bring down inflammation.
Spinach
Spinach and other leafy green vegetables are a common suggestion for someone suffering from this condition. Pancreatitis is often worsened by vitamin deficiency, specifically vitamin A, vitamin E, and vitamin C, as well as selenium. Fortunately, these essential nutrients can all be sourced in spinach, so don’t be afraid to load up a salad and enjoy the quick relief!
Coconut Oil
When cooking, you should avoid the use of traditional vegetable oils if possible, as the fat content is not helpful for pancreatitis. However, coconut oils and other alternative cooking oils are much healthier, and have a better balance of omega-3 and omega-6 fatty acids, helping prevent the inflammation of this condition.
Red Grapes
Another powerful antioxidant that has been shown to work well against pancreatitis is resveratrol, which is found in high concentrations in red grapes. Not only is this a delicious remedy, but also a highly effective one!
Medicinal Herbs for Pancreatitis:
Herbal remedies for pancreatitis consist of many effective organic components that have a multi-target effect on the disease.
Experiments on animals found that these herbal formulas have a significant impact and that they can be used as an adjunctive treatment for pancreatitis.
Follow-up studies on patients with pancreatitis showed that these remedies are effective in treating both acute and chronic pancreatitis.
Cinnamon:
Cinnamon (Cinnamomum Verum) is a multifaceted medicinal plant that has anti-inflammatory, anti-diabetic, and antimicrobial properties. It also has lipid-lowering activities, protects against neurological disorders such as Parkinson’s and Alzheimer’s diseases, and lowers the risk of cardiovascular disease.
Cinnamon is also used in traditional medicine to prevent and treat pancreatitis – in fact, cinnamon is the key ingredient in a Chinese herbal Medicine for pancreatitis known as Guizhi Decoction.
The essential oils from cinnamon may provide a protective effect on pancreatic beta cells and ameliorate oxidative stress. Eugenol, an oil found in cinnamon may also help to prevent pancreatitis-induced acute kidney injury.
To use cinnamon for pancreatitis, add 2 or 3 sticks of cinnamon to a glass of boiling hot water. Stir it for 15-30 seconds and then set it aside to steep.
When the tea is still warm, add a little lemon juice and honey to taste. You can also mix half a teaspoon of cinnamon powder with a tablespoon of honey and consume this instead of the tea.
Peony:
The peony root (Paeonia Officinalis) was used by ancient Chinese and Japanese doctors to treat convulsions. Red and white peony root extracts are also used to treat liver cirrhosis, menstrual cramps, and muscle cramps.
Studies show that red peony root is an effective treatment for severe acute pancreatitis as it helps to reduce the fever, abdominal tenderness, and abdominal distension associated with this condition.
Furthermore, this remedy can be used along with allopathic medications such as anti-bacterial and anti-fungal agents to reduce treatment time. Similarly, white peony root can be used to treat acute pancreatitis as it has a relaxing effect on the sphincter of Oddi which controls the flow of bile and pancreatic juice from the pancreas to the small intestine.
Pancreatitis causes elevated levels of an enzyme called pancreatic amylase; since white peony inhibits pancreatic amylase, an herbal formulation with this ingredient can bring about quick results.
Peony is one of the main ingredients of traditional Chinese medicine called Bupleurium-Peony Cheng Qi which is used to treat pancreatitis.
To use peony root for pancreatitis, you will need to add the peony root to boiling water and allow it to simmer (not boil) for 20 minutes before taking it off the stove. Let the decoction steep until it is cool enough to drink.
Rhubarb:
Chinese rhubarb was one of the first Chinese medicinal herbs to be imported to the West from China. While rhubarb leaves are toxic, the stems and roots are rich in therapeutic organic compounds called anthraquinones.
Animal studies show that rhubarb extract reduced the serum amylase and tumor necrosis factor levels in rats with acute pancreatitis.
Similar studies on the effects of rhubarb on pancreatitis found that rhubarb can have a protective effect on severe acute pancreatitis by inhibiting the inflammation of the pancreas.
Rhubarb can also reduce pancreatic tissue damage caused by pancreatitis. It can also promote the proliferation of pancreatic acinar cells that secrete and store digestive enzymes.
Rhubarb could promote pancreatic regeneration which would enhance recovery. Rhubarb can also be used along with conventional medications for pancreatitis such as somatostatin and trypsin inhibitors to shorten the recovery period, reduce abdominal pain quickly, and even decrease the mortality risk.
Rhodiola:
Rhodiola (Rhodiola Rosea) also known as roseroot has been used for centuries as a traditional medication for stress, depression, and anxiety.
Reviews in 2011 and 2012 found that this herb can reduce mental fatigue as well as enhance physical performance due to its adaptogen properties.
However, recent studies found that roseroot may also be effective in the treatment of pancreatitis. Animal models showed that roseroot can help prevent renal damage in cases of severe acute pancreatitis.
Roseroot helps to regulate enzyme production in the pancreas as well as reduce the generation of free radicals which improves kidney function.
Roseroot is available as a liquid extract, a dried powder, or even in the form of capsules and tablets which makes it easy to include it in your pancreatitis treatment plan.
Dandelion Root:
Pancreatitis and diabetes are closely linked to each other as studies show that chronic inflammation of the pancreas can damage the insulin-producing cells within the pancreas which can lead to diabetes
On the flip side, people with diabetes have a twofold to threefold increased risk of suffering from pancreatitis.
Studies on dandelion root extract (Taraxacum officinale) show that it can help to stimulate the release of insulin which helps to stabilize blood sugar levels. It also increases glucose uptake by muscle cells and has anti-inflammatory properties which can help to prevent pancreatitis.
It also increases glucose uptake by muscle cells and has anti-inflammatory properties which can help to prevent pancreatitis. People who suffer from chronic pancreatitis have an increased risk of pancreatic cancer.
Preliminary studies indicate that dandelion root extract can help to destroy human pancreatic cancer cells with no negative effect on noncancerous cells.
The simplest way to include dandelion root in your recovery plan is to clean and dry the fresh root and then use this powder to make fresh dandelion root tea.
Other Medicinal Herbs for Pancreatitis
- Licorice (Glycyrrhiza glabra)
- Calendula (Calendula officinalis)
- Goldenseal (Hydrastis Canadensis)
- Horsetail (Equisetum arvense)
- Oregano (Origanum vulgare)
- Turmeric (Curcuma longa)
Medicinal Herbs. Catalog and prices
Artificial pancreas:
When a person’s pancreas isn’t functioning properly or has to be removed, doctors may replace or supplement it with an artificial pancreas. These devices that automatically monitor blood glucose and provide the appropriate insulin doses are often called closed-loop systems, automated insulin delivery systems, or autonomous systems for glycemic control, according to the Food and Drug Administration.
In a 2014 study published in the journal The Lancet Diabetes & Endocrinology, researchers found that an artificial pancreas offers people with type 1 diabetes a reliable way to keep glucose levels in check when compared to other treatments. “Our study confirms that both artificial pancreas systems improve glucose control and reduce the risk of hypoglycemia compared to conventional pump therapy,” study author Ahmad Haidar, of Institut de Recherches Cliniques de Montreal, said in a statement.
Personal Note:
I am not a big fan of, “Big Pharma” but always follow your Doctor’s recommendations first.
Thank you for reading.
Michael
Comments are welcome
I was recently diagnosed with type 2 diabetes. My Dr. explained it to me that the pancreas is failing at it’s job. I haven’t done a whole lot of research on it, but I am starting to now. My search for pancreas problems brought me to your website. I was wondering if you had any homeopathic suggestions I could research?
Hi Adam,
Thank you for your comments. I am sorry to hear about you being diagnosed with type 2 diabetes and the reasons for the diagnosis. I do not have anything on homeopathic remedies. I did publish an article on diabetes 2 on my site also. Not sure if it is OK to publish the URL related to that specific post. One way to find out:
https://empoweryourlifestyles….
Hope you find something helpful and wish you the best of health.
Michael
thanks for the list of herbal medicines for pancreatic diseases . Appreciate this
Hi Fitoru,
Thank you for your comments. Glad you found the list of herbal remedies helpful. Please remember seeing a Doctor is essential.
Best wishes,
Michael