What is Emphysema?
Blue indicates link
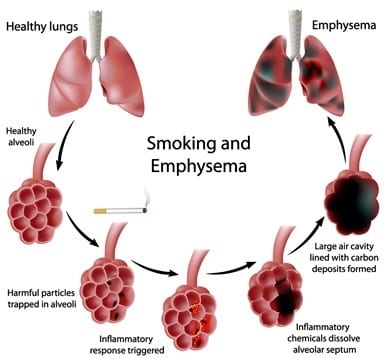
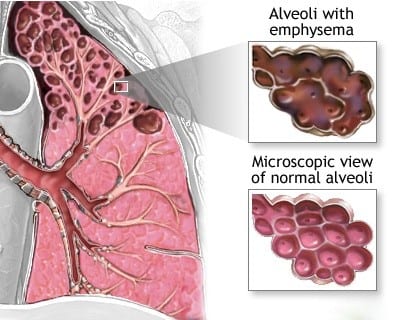
Emphysema is a lung condition that causes shortness of breath. In people with emphysema, the air sacs in the lungs (alveoli) are damaged. Over time, the inner walls of the air sacs weaken and rupture — creating larger air spaces instead of many small ones. This reduces the surface area of the lungs and, in turn, the amount of oxygen that reaches your bloodstream.
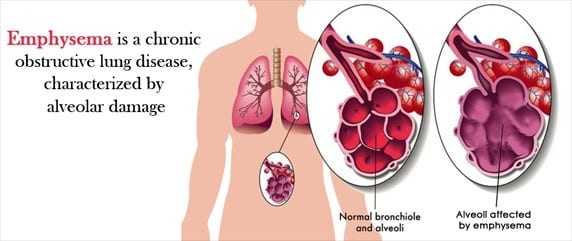
When you exhale, the damaged alveoli don’t work properly and old air becomes trapped, leaving no room for fresh, oxygen-rich air to enter.
Most people with emphysema also have chronic bronchitis. Chronic bronchitis is inflammation of the tubes that carry air to your lungs (bronchial tubes), which leads to a persistent cough.
Emphysema and chronic bronchitis are two conditions that make up chronic obstructive pulmonary disease (COPD). Smoking is the leading cause of COPD. Treatment may slow the progression of COPD, but it can’t reverse the damage.
Symptoms:
You can have emphysema for many years without noticing any signs or symptoms. The main symptom of emphysema is shortness of breath, which usually begins gradually.
You may start avoiding activities that cause you to be short of breath, so the symptom doesn’t become a problem until it starts interfering with daily tasks. Emphysema eventually causes shortness of breath even while you’re at rest.
Causes:
The main cause of emphysema is long-term exposure to airborne irritants, including:
- Tobacco smoke
- Marijuana smoke
- Air pollution
- Chemical fumes and dust
Rarely, emphysema is caused by an inherited deficiency of a protein that protects the elastic structures in the lungs. It’s called alpha-1-antitrypsin deficiency emphysema.
Doctors describe how bad your emphysema is by using what they call “stages.” They use two main methods to come up with this information — the GOLD Emphysema Staging System and the BODE Index. Read on to learn more about each of them.
The GOLD Emphysema Staging System.
This is a set of guidelines established by the Global Initiative for Chronic Obstructive Lung Disease (GOLD).
It measures how much air you can blow out of your lungs in 1 second. Doctors call this the forced expiratory volume (FEV1).
If you have emphysema, your doctor will look at your FEV1. He’ll also look at your other symptoms, as well as how many times you’ve been hospitalized in the past year because of them. Doctors call this an “exacerbation.” It means your symptoms flare up or suddenly get worse.
Your doctor may also do a CT scan of your lungs. He’ll then use all of this information to place you into one of the following four groups (they tell you how severe your emphysema is):
Group A (GOLD 1 or 2):
Your symptoms are very mild. Your FEV1 is 80% or more. You might have had no flare-ups over the past year, or perhaps just one. You weren’t hospitalized for your symptoms.
Group B (GOLD 1 or 2):
Your FEV1 is between 50% and 80%. You have more symptoms than people in Group A. This is the stage where most people see their doctor for coughing, wheezing, and shortness of breath.
You might have had one major flare-up, but you haven’t been in the hospital for your symptoms within the past year.
Group C (GOLD 3 or 4):
Airflow into and out of your lungs is severely limited. Your FEV1 is between 30% and 50%.
You’ve had more than two flare-ups in the past year, or you’ve been admitted to the hospital at least once.
Group D (GOLD 3 or 4):
It’s extremely hard for you to breathe in or out. You’ve had at least two flare-ups in the past year, or you’ve been hospitalized at least once.
Doctors call this “end-stage” COPD. That means you have very little lung function. Any new flare-ups could be life-threatening.
The BODE Index:
This staging system measures how much emphysema impacts your daily life. It looks at four main areas:
Body mass index (B).
This describes how much body fat you have compared to your height and weight.
Airflow limitation (O for obstruction).
Your doctor can tell how damaged your lungs are by how well you do on pulmonary (lung) function tests.
Breathlessness (D – doctors call it “dyspnea”).
Your doctor will ask you a series of questions about how often you feel like you’re out of breath, and when.
Exercise capacity (E).
This measures how far you can walk in 6 minutes.
Studies show that the BODE Index gives doctors a better idea about your outcome (what they call a “prognosis”) than FEV1. And they can use those findings to see how well you’ll respond to medications, lung rehab therapy, and other treatments.
Emphysema gets worse over time, and it affects everyone differently. That means there’s no way doctors can know for sure how long you can expect to live if you have it.
Your doctor will use information about the stage of your disease to come up with the best treatment plan for your special case.
How do Doctors Determine If You Have Emphysema?
Your chest feels tight, you’re out of breath much of the time, and you have a cough that won’t go away. Do you have emphysema? You can’t go on symptoms alone. See your doctor.
He’ll do the following tests to find out for sure:
Medical History:
Your doctor will talk to you about your health and any recent changes you might have noticed. If you have emphysema, you’ll probably have had shortness of breath, often over a period of months or years. You may also experience wheezing. You might have a cough that won’t go away, too.
Physical Exam:
Your doctor will check your weight and blood pressure. He’ll listen to your heartbeat and keep an eye out for anything that seems strange or unusual.
If you have advanced emphysema, your doctor may notice that you have any of the following:
- You have a “barrel chest” caused by larger-than-normal lungs.
- You’re wheezing, and having a hard time getting air out of your lungs.
- Your fingertips are rounded. Doctors call this “clubbing.”
- You purse your lips when you breathe like you’re blowing a kiss.
- The oxygen levels in your blood are low (hypoxemia).
- The carbon dioxide levels in your blood are high (hypercarbia) because emphysema makes it hard to exhale properly.
- Your lips have a blue tinge (cyanosis), another sign of low oxygen in your blood.
- Malnutrition causes muscles to slowly waste away in advanced emphysema.
Pulmonary Function Tests (PFTs)
For this exam, you may sit inside an enclosed booth and breathe into a tube. This will allow your doctor to measure:
- How much air your lungs can hold
- How fast you can blow air out of your lungs
- How much air stays trapped in your lungs after you exhale
- Whether you’re able to breathe better after using medicines you inhale, such as albuterol
If you have normal lungs, you’ll likely be able to empty most of the air from them in 1 second. If you have emphysema, it’ll probably take longer.
Chest X-ray and CT Scan:
If you have advanced emphysema, your lungs will appear to be much larger than they should be. In the early stages of the disease, your chest X-ray may look normal. Your doctor can’t diagnose emphysema with an X-ray alone.
A CT scan of your chest will show if the air sacs (alveoli) in your lungs have been destroyed. These make it hard for you to breathe out like normal.
Complete Blood Count:
This simple blood test usually shows normal amounts of white and red blood cells. In advanced emphysema, your body produces more red blood cells to make up for decreased oxygen. These cells carry oxygen.
If your white blood cell count is higher than normal, that’s a possible sign of infection.
Treatments For Emphysema:
Emphysema can’t be cured, but there are a number of treatments that relieve symptoms by making it easier for you to breathe. They can also prevent other problems and keep the disease from getting worse.
This article deals with some of the most common treatments. What your doctor recommends will depend on how severe your symptoms are.
Bronchodilators
These drugs relieve symptoms by relaxing the muscles in the lungs and making the air passages wider. Bronchodilators often use an inhaler (“puffer”). They also come in pill or liquid form, but these don’t work as well as an inhaler, and they can have more side effects.
There are short-acting and long-acting bronchodilators. The short-acting drugs work faster but don’t last as long. The long-acting ones don’t work as fast, but they last longer. If your emphysema symptoms are mild, your doctor may recommend you take short-acting bronchodilators during flare-ups. As your symptoms get worse, you may have to take daily doses of long-acting bronchodilators.
Bronchodilators come in two forms:
- Anticholinergics stop the muscles around your airways from tightening. They also make it easier to clear mucus from the lungs.
- Beta-agonists relax muscles around the airways.
Your doctor may prescribe short-acting beta-agonists only when you need them, to control your symptoms. They start working within 3 to 5 minutes and last 4 to 6 hours. But they may cause your heart to race. They can also cause shakiness and cramping in the hands, legs, and feet. These side effects can make you feel anxious. That, in turn, can make it harder for you to breathe.
Short-acting anticholinergics start working in about 15 minutes and last 6 to 8 hours. Long-acting forms of these drugs can take about 20 minutes to work and last up to 24 hours. The most common side effects of these drugs are dry mouth and difficulty peeing.
If you have advanced emphysema, your doctor may prescribe a long-acting inhaled bronchodilator. They’re used on a regular schedule to open your airways and keep them open.
PDE-4 Inhibitors:
Newer oral drugs called phosphodiesterase-4 (PDE-4) inhibitors have also proved to work in treating chronic obstructive pulmonary disease (COPD).
A number of clinical trials showed the PDE-4 drug Roflumilast improved lung function when used with bronchodilator therapy. Some studies found it also led to fewer flare-ups.
The FDA approved Roflumilast for bronchitis, not emphysema, but the two conditions often have similar symptoms.
Steroids and Combination Medicines
Steroids reduce swelling and mucus in your airways so you can breathe easier. Usually, you breathe them in with an inhaler.
Over time, steroids can have serious side effects, including weight gain, diabetes, cataracts, high blood pressure, weakened bones, and an increased risk of infection.
Your doctor may recommend you use steroids along with beta-agonists or anticholinergic bronchodilators. This provides more benefits than using either drug alone. It’s also easier because you have one inhaler instead of two.
Mucolytics
These drugs help thin the mucus in your lungs so you can cough it up more easily. Studies show using them can reduce flare-ups, especially if your emphysema is more severe.
Protein Therapy
Some people have an inherited form of emphysema that’s caused by a lack of the protein alpha-1 antitrypsin (AAT). Getting infusions of AAT can help slow down lung damage.
Oxygen Therapy
As your emphysema progresses, you may need extra oxygen to help you breathe on your own. Your doctor will prescribe how much oxygen you need and when you should be taking it. You can take supplemental oxygen in one of the following three ways:
- Oxygen concentrator. This device removes other gases from the air and gives you near-pure oxygen. (Air normally contains 21% oxygen.)
- Liquid system. This is supercooled, pure oxygen stored in a canister that looks like a thermos.
- Oxygen cylinders. These contain 100% oxygen, stored under high pressure in large or small tank-like containers.
Vaccines
The flu vaccine doesn’t treat emphysema directly, but doctors recommend you get one every year. They also suggest you get a pneumonia shot every 5 to 7 years to prevent infection. If you have emphysema, you have higher odds of serious problems from flu and pneumonia.
Surgery
There are a number of different types of operations for more serious cases of emphysema. They include:
- Lung volume reduction surgery (LVRS). In this procedure, a surgeon removes part of one or both of your lungs. The goal is to take out your nonworking air sacs so it’s easier to breathe. This is major surgery, so your heart has to be strong and the rest of your lungs need to be healthy before you can have it. You’ll also need to quit smoking and complete a pulmonary rehabilitation program before the operation.
- Bullectomy. In rare cases, air sacs in the lungs caused by emphysema grow larger and can press against healthy parts of the lung. These oversized sacs are called bullae. A bullectomy is a surgery to remove them.
- Lung Transplant. Lung transplants are possible for the most severe cases. This is a 6- to 10-hour surgery, after which you’ll be in the hospital for 8 to 21 days — if there are no complications. The two biggest risks of the operation are infection and rejection of the transplanted organ.
- New Treatments on the Horizon
Researchers are developing ways to treat severe cases of emphysema without major surgery. They include:
- One-way valves. In this procedure, the doctor places valves in diseased parts of the lung. The valves block airflow and mucus to those areas so the healthy areas of the lung can work better.
- Lung volume reduction coil treatment (LVRC). The doctor inserts straightened nickel-titanium coils into the lungs. There, they act as a spring that pulls together diseased areas, making them smaller. As with the one-way valve, the goal is to allow the healthy parts of the lung to work better.
- Bronchoscopic thermal vapor ablation (BVTA). This procedure reduces lung volume by using heated water vapor to cause scarring. It’s designed for people who have severe emphysema in the upper lobes of their lungs.
- Airway bypass. Doctors place a stent, or tube, into severely diseased airways, allowing air that’s trapped in the lungs to escape. The stent also contains the drug paclitaxel to stop tissue growth inside the airways.
- Targeted lung denervation (TLD). Researchers are also looking at removing certain nerves around the airways with this procedure. It targets nerves that make your muscles contract and produce too much mucus. A small pilot study found TLD was safe. Patients showed improvements, but researchers say more study is needed into this technique.
Risk factors:
 Factors that increase your risk of developing emphysema include:
Factors that increase your risk of developing emphysema include:
Smoking. Emphysema is most likely to develop in cigarette smokers, but cigar and pipe smokers also are susceptible. The risk for all types of smokers increases with the number of years and the amount of tobacco smoked.
- Age. Although the lung damage that occurs in emphysema develops gradually, most people with tobacco-related emphysema begin to experience symptoms of the disease between the ages of 40 and 60.
- Exposure to secondhand smoke. Secondhand smoke, also known as passive or environmental tobacco smoke, is smoke that you inadvertently inhale from someone else’s cigarette, pipe, or cigar. Being around secondhand smoke increases your risk of emphysema.
- Occupational exposure to fumes or dust. If you breathe fumes from certain chemicals or dust from grain, cotton, wood, or mining products, you’re more likely to develop emphysema. This risk is even greater if you smoke.
- Exposure to indoor and outdoor pollution. Breathing indoor pollutants, such as fumes from heating fuel, as well as outdoor pollutants — car exhaust, for instance — increases your risk of emphysema.
Complications:
People who have emphysema are also more likely to develop:
- Collapsed lung (pneumothorax). A collapsed lung can be life-threatening in people who have severe emphysema because the function of their lungs is already compromised. This is uncommon but serious when it occurs.
- Heart problems. Emphysema can increase the pressure in the arteries that connect the heart and lungs. This can cause a condition called cor pulmonale, in which a section of the heart expands and weakens.
- Large holes in the lungs (bullae). Some people with emphysema develop empty spaces in the lungs called bullae. They can be as large as half the lung. In addition to reducing the amount of space available for the lung to expand, giant bullae can increase your risk of pneumothorax.
Curing Emphysema Naturally:
Anti-Emphysema Diet:
A person suffering from emphysema must eat only fruits and vegetables for at least a week during the start of treatment. Preferably, only drink fruit juices for the first two days and then follow with eating fresh green vegetables and fruits like pineapple, orange, pear, papaya, peach, and apple. Also, remember to administer a water enema every early morning for a week to keep the bowels clean. The fruit and vegetable diet must be adopted every two months if conditions do not improve.
Do not boil the vegetables. Try to consume raw. Eat nuts, whole grains, goat milk, buttermilk, curd, and vegetable oil on other days. Avoid using too much salt in food if you suffer from emphysema. Sodium in common salt leads to inflammation of bronchial passages causing breathlessness and leading to serious damage in the lungs.
Garlic:
The juice of garlic is beneficial in clearing the air passages in the lungs. Chew two to three cloves of garlic on an empty stomach every day. If you cannot bear the pungent odor, use large portions of garlic in cooking extract the juice and use it as a salad dressing, or mix it with other fruit and vegetable juices.
Aniseed:
Aniseed has expectorant properties which help to reduce the swelling of the alveoli caused by emphysema. Extract aniseed oil and mix 10 to 15 drops of it in brown sugar. Take two teaspoons of this mixture twice a day to cure emphysema.
Lemon Juice:
The anti-inflammatory properties of vitamin C in fresh lime juice restore the elasticity of lung tissues and thus reduce swelling. Sip on fresh lime juice during and in between meals. Do not add salt to the lime juice; however, honey or sugar can be added.
Serrapeptase:
This is a form of herbal extract that helps to cure blood clots, plaque in the artery, and lung inflammation. Consumption of this extract will thus help to clear the air passage and cure emphysema.
Amaranth:
This is another green leafy herb widely used to treat patients with lung diseases. The fresh juice of amaranth can be mixed with honey or brown sugar and taken by the patient anytime during the day. The juice helps to restore the biochemical balance in human blood.
Smoke fills in the lungs and causes an obstruction for fresh air to get in. Without the availability of adequate oxygen, people experience breathlessness. Passive smoking is also not good for emphysema patients. Try to live in a smoke-free environment and breathe in the necessary amount of air through oxygen cylinders.
Personal Note:
We are living in a world that is being attacked by respiratory diseases. Some of these diseases can be prevented as outlined in the article. My father suffered from emphysema and he was forced to quit smoking so he could live. It is not a good feeling when you are struggling to breathe.
Thank you for reading,
Michael
Comments are welcome.
I found it interesting that there are eating restrictions that go along with emphysema. I always thought this was a disease for smokers, so I was surprised to see that you can get this even if you don’t smoke. It gives us all just one more reason to limit our exposure to environmental toxins and stay as healthy as possible.
Hi Theresa,
Thank you for your comments. The list of respiratory illness is staggering, the latest being COVID-19. Environmental toxins are the 4th leading cause of death according to recent studies.
Stay safe and healthy,
Michael
This is a very indepth post with valuable information. I now have a far greater understanding for the lung condition of emphysima so thank you. As somebody who spent years as a smoker I am glad that I stopped this bad habbit and now feel considerably better for doing so.
I had no idea of a natural cure to the problem and will bookmark this page for future reference before my next weekly shop.
eA very insteresting post and thank you.
Hi Mike,
Thank you for your comments. Congratulations on quitting smoking. There are so many respiratory diseases out there, the most recent COVID-19. Wishing you a healthy safe life.
All the best,
Michael
After years of working in construction and smoking cigarettes, I was diagnosed with COPD and pulmonary fibrosis. As my illness progressed, I found myself relying on supplemental oxygen around the clock. Even getting out of bed became a challenge. My doctors and specialists recommended a lung transplant, but after researching the pros and cons of such a drastic procedure, I decided to try something less invasive. I contacted multivitamin herbal cure cape town for organic natural treatment you can search for them on google. Following the COPD and pulmonary fibrosis herbal treatment procedure, my lung function has improved dramatically after my first four weeks of the herbal formula. My quality of life has gotten a lot better. I was amazed that I could breathe without any dead air. I no longer need oxygen and look forward to continued improvement because a specialist told me already I have a 97% chance of getting my condition totally due to the herbal treatment effectiveness.
I was constantly tired and short of breath due to my Emphysema, I was introduced to VineHealth Center and their COPD Herbal Protocol. I started on the COPD Treatment last year, my symptoms gradually diminished including my shortness of breath, wheezing and fatigue.
Rhonda S.’s COPD made her feel short of breath and like she was constantly dragging. While her inhalers helped some, she just didn’t feel like herself anymore.
After having life-threatening pneumonia, she knew something had to change. A friend of hers mentioned multivitamin herbal formula restoration treatment, so Rhonda did
some research and decided to receive treatment at the multivitamin herbal cure. “I started to feel better almost right away,” Rhonda said.
And, along with feeling better, she began to do things she couldn’t do before treatment. Now, Rhonda can take showers, work in her flower garden, and she enjoys having more energy. It’s with a great deal of hope, Rhonda says, “I feel more like myself.”
Like Rhonda, you can breathe easier and bring normal life back within reach.
In 2015, my best friend Linda was diagnosed with end-stage chronic obstructive pulmonary disease (COPD) during a hospital visit, and that diagnosis would change her life in many ways. She had to use supplemental herbal formulas, and she wasn’t able to walk 10 feet down the hall or do routine chores like cooking and cleaning.
Linda decided to take a chance on the herbal cure. About 4 weeks after treatment, she got up to do something, and she felt so good that she moved on to another task. Several hours later, Linda realized that she’d been doing all these tasks without any oxygen at all. She’s also happy to be able to talk to people on the phone without a lot of huffing and puffing. These days, she can once again participate in one of her favorite activities: fishing on her pontoon boat. Linda wants other people with COPD to know. Don’t give up!”
Thank you for the share. Glad to hear Linda is doing well.
Best wishes,
Michael
I had emphysema in 2009 when I was 45 years old. I smoked for 11 years, but quit smoking as soon as I was told that I had COPD. Quitting smoking was the hardest thing I ever did. But I knew I would die if I didn’t. My health was getting so bad that I needed oxygen 24/7 and was down to 92lbs. Thankfully, in 2019 I got a natural herbal prescription from a friend. It saved my life. I no longer needed oxygen and was able to climb stairs, dance, and travel the world.This is their website www multivitamincare org
I had emphysema in 2009 when I was 45 years old. I smoked for 11 years, but quit smoking as soon as I was told that I had COPD. Quitting smoking was the hardest thing I have ever done. But I knew I would die if I didn’t. My health was getting so bad that I needed oxygen 24/7 and was down to 92lbs. Thankfully, in 2019 I got a natural herbal prescription from a friend. It saved my life. I no longer needed oxygen and was able to climb stairs, dance, and travel the world. This is their website www multivitamincare org
Hi Jacob, I am glad and congratulate you on quitting smoking. I appreciate you sending me the site.
Climbing stairs, and traveling the world that is awesome. Please take care of yourself.
Michael