The Coronaviruses. History and Present
Blue indicates link
Coronaviruses are types of viruses that typically affect the respiratory tract of mammals, including humans. They are associated with the common cold, pneumonia, and severe acute respiratory syndrome (SARS) and can also affect the gut.
A coronavirus was first isolated in 1937 from an infectious bronchitis virus in birds that have the ability to seriously devastate poultry stocks.
These viruses are responsible for between 15 and 30 percent of common colds.
Over the last 70 years, scientists have found that coronaviruses can infect mice, rats, dogs, cats, turkeys, horses, pigs, and cattle.
This MNT Knowledge Center article will focus on the different types of human coronaviruses, their symptoms, how they are transmitted, and two particularly dangerous diseases that can be caused by coronaviruses: SARS and MERS.
Fast facts on coronaviruses:
There is no cure for the common cold.
A coronavirus causes both SARS and MERS.
Coronaviruses infect many different species.
There are six known human coronaviruses.
SARS spread from China to cause infection in 37 countries, killing 774 people.
What are corona-viruses?
Coronaviruses can cause flu-like symptoms and respiratory symptoms.
Human coronaviruses (HCoV) were first identified in the 1960s in the noses of patients with the common cold. Two human coronaviruses are responsible for a large proportion of common colds OC43 and 229E.
Coronaviruses were given their name based on the crown-like projections on their surfaces. “Corona” in Latin means “halo” or “crown.”
Among humans, the infection most often occurs during the winter months as well as early spring. It is not uncommon for a person to become ill with a cold that is caused by a coronavirus and then catch it again about four months later.
This is because coronavirus antibodies do not last for a very long time. Also, the antibodies for one strain of the coronavirus may be useless against other strains.
Symptoms
Symptoms include:
sneezing
a runny nose
fatigue
a cough
In rare cases, fever
a sore throat
exacerbated asthma
Human coronaviruses cannot be cultivated in the laboratory easily, unlike the rhinovirus, another cause of the common cold. This makes it difficult to gauge the coronavirus’s impact on national economies and public health.
There is no cure, so treatments include taking care of yourself and over-the-counter (OTC) medication:
Rest and avoid overexertion.
Drink enough water.
Avoid smoking and smoky areas.
Take acetaminophen, ibuprofen, or naproxen to reduce pain and fever.
Use a clean humidifier or cool mist vaporizer.
The virus responsible can be diagnosed by taking a sample of respiratory fluids, such as mucus from the nose, or blood.
Types:
Different types of human coronaviruses vary in the severity of the illness they cause and how far they can spread.
There are currently six recognized types of coronavirus that can infect humans.
Common types include:
229E (alpha coronavirus)
NL63 (alpha coronavirus)
OC43 (beta coronavirus)
HKU1 (beta coronavirus)
Rarer, more dangerous types include MERS-CoV, which causes Middle East Respiratory Syndrome (MERS), and severe acute respiratory syndrome (SARS-CoV), the coronavirus responsible for SARS.
Transmission
Contagious diseases can spread through coughing without covering the mouth.
There has not been a great deal of research on how a human coronavirus spreads from one person to the next.
However, it is believed that viruses are transmitted using secreted fluid from the respiratory system.

Coronaviruses can spread in the following ways:
Coughing and sneezing without covering the mouth can disperse droplets into the air, spreading the virus.
Touching or shaking hands with a person who has the virus can pass the virus from one person to another.
Making contact with a surface or object that has the virus and then touching your nose, eyes, or mouth.
On rare occasions, a coronavirus may spread through contact with feces.
People in the U.S. are more likely to contract the disease in the winter or fall. The disease is still active during the rest of the year. Young people are most likely to contract a coronavirus, and people can contract more than one infection over the course of a lifetime. Most people will become infected with at least one coronavirus in their life.
Centers for Disease Control and Prevention
It is said that the mutating abilities of the coronavirus are what make it so contagious.
To prevent transmission, be sure to stay at home and rest while experiencing symptoms and avoid close contact with other people. Covering the mouth and nose with a tissue or handkerchief while coughing or sneezing can also help prevent the spread of the coronavirus. Be sure to dispose of any used tissues and maintain hygiene around the home.
SARS
Severe acute respiratory syndrome (SARS) was a contagious disease caused by the SARS-CoV coronavirus. It typically led to a life-threatening form of pneumonia.
The virus started off in the Guangdong Province in southern China in November 2002, eventually reaching Hong Kong. From there, it rapidly spread around the world, infecting people in 37 countries.
SARS-CoV is unique. It can infect both the upper and lower respiratory tract and can also cause gastroenteritis.
The symptoms of SARS develop over the course of a week and start with a fever. Early on in the condition, people develop flu-like symptoms, such as:
dry coughing
chills
diarrhea
breathlessness
aches
Pneumonia, a severe lung infection, may develop afterward. At its most advanced stage, SARS causes failure of the lungs, heart, or liver.
During the epidemic, there were 8,098 confirmed cases of SARS with 774 fatalities. This is equal to a mortality rate of 9.6 percent. Complications were more likely in older adults, and half of all infected people over the age of 65 years who became ill did not survive. It was eventually brought under control in July 2003.
MERS
MERS is a potentially fatal coronavirus.
MERS, caused by the MERS-CoV coronavirus, was first recognized in 2012. This severe respiratory illness first surfaced in Saudi Arabia and, since then, has spread to other countries. The virus has reached the U.S., and the largest outbreak outside the Arabian Peninsula occurred in South Korea in 2015.
Symptoms include fever, breathlessness, and coughing. The illness spreads through close contact with people who have already been infected. However, all cases of MERS are linked to individuals who have recently returned from travel to the Arabian Peninsula.
MERS is fatal in 30 to 40 percent of people who contract it.
Medically reviewed by Daniel Murrell, M.D. on February 1, 2018 — Written by Adam Felman
History
The history of human coronaviruses began in 1965 when Tyrrell and Bynoe1 found that they could pass a virus named B814. It was found in human embryonic tracheal organ cultures obtained from the respiratory tract of an adult with a common cold. The presence of an infectious agent was demonstrated by inoculating the medium from these cultures intranasally in human volunteers; colds were produced in a significant proportion of subjects, but Tyrrell and Bynoe were unable to grow the agent in tissue culture at that time.
At about the same time, Hamre and Procknow2 were able to grow a virus with unusual properties in tissue culture from samples obtained from medical students with colds. Both B814 and Hamre’s virus, which she called 229E, were ether-sensitive and therefore presumably required a lipid-containing coat for infectivity, but these 2 viruses were not related to any known myxo- or paramyxoviruses.
While working in the laboratory of Robert Chanock at the National Institutes of Health, McIntosh et al3 reported the recovery of multiple strains of ether-sensitive agents from the human respiratory tract by using a technique similar to that of Tyrrell and Bynoe. These viruses were termed “OC” to designate that they were grown in organ cultures.
Within the same time frame, Almeida and Tyrrell4 performed electron microscopy on fluids from organ cultures infected with B814 and found particles that resembled the infectious bronchitis virus of chickens. The particles were medium-sized (80–150 nm), pleomorphic, membrane-coated, and covered with widely spaced club-shaped surface projections. The 229E agent identified by Hamre and Procknow2 and the previous OC viruses identified by McIntosh et al3 had similar morphology.
In the late 1960s, Tyrrell was leading a group of virologists working with human strains and a number of animal viruses. These included infectious bronchitis virus, mouse hepatitis virus, and transmissible gastroenteritis virus of swine, all of which had been demonstrated to be morphologically the same as seen through electron microscopy. This new group of viruses was named coronavirus (corona denoting the crown-like appearance of the surface projections) and was later officially accepted as a new genus of viruses.
Ongoing research using serologic techniques has resulted in a considerable amount of information regarding the epidemiology of human respiratory coronaviruses. It was found that in temperate climates, respiratory coronavirus infections occur more often in the winter and spring than in the summer and fall. Data revealed that coronavirus infections contribute as much as 35% of the total respiratory viral activity during epidemics. Overall, the proportion of adult colds produced by coronaviruses was estimated at 15%.8
In the 3 decades after discovery, human strains OC43 and 229E were studied exclusively, largely because they were the easiest ones to work with. OC43, adapted to growth in the suckling mouse brain and subsequently to tissue culture, was found to be closely related to the mouse hepatitis virus. Strain 229E was grown in tissue culture directly from clinical samples.
The 2 viruses demonstrated periodicity, with large epidemics occurring at 2- to 3-year intervals, .9 Strain 229E tended to be epidemic throughout the United States, whereas strain OC43 was more predisposed to localized outbreaks. As with many other respiratory viruses, reinfection was common. The infection could occur at any age, but it was most common in children.
Despite the extensive focus placed exclusively on strains 229E and OC43, it was clear that there were other coronavirus strains as well. As shown by Bradburne,11 coronavirus strain B814 was not serologically identical with either OC43 or 229E. Contributing to the various strain differences in the family of coronaviruses, McIntosh et al12 found that 3 of the 6 strains previously identified were only distantly related to OC43 or 229E.
Epidemiologic and volunteer inoculation studies found that respiratory coronaviruses were associated with a variety of respiratory illnesses; however, their pathogenicity was considered below.2,8,13,14 The predominant illness associated with infections was an upper respiratory infection with occasional cases of pneumonia in infants and young adults.15,16 These viruses were also shown to be able to produce asthma exacerbations in children as well as chronic bronchitis in adults and the elderly.
While the research was proceeding to explore the pathogenicity and epidemiology of human coronaviruses, the number and importance of animal coronaviruses were growing rapidly. Coronaviruses were described as causing disease in multiple animal species, including rats, mice, chickens, turkeys, calves, dogs, cats, rabbits, and pigs. Animal studies included, but were not limited to, research that focused on respiratory disorders. The study focus included disorders such as gastroenteritis, hepatitis, and encephalitis in mice; pneumonitis and sialodacryoadenitis in rats; and infectious peritonitis in cats.
The interest peaked particularly regarding areas of encephalitis produced by mouse hepatitis virus and peritonitis produced by infectious peritonitis virus in cats. The pathogenesis of these disease states was various and complex, demonstrating that the genus as a whole was capable of a wide variety of disease mechanisms.20 Human and animal coronaviruses were segregated into 3 broad groups based on their antigenic and genetic makeup. Group, I contained virus 229E and other viruses, group II contained virus OC43, and group III was made up of avian infectious bronchitis virus and a number of related avian viruses.
Given the enormous variety of animal coronaviruses, it was not surprising when the cause of a very new, severe acute respiratory syndrome, called SARS, emerged in 2002–2003 as a coronavirus from southern China and spread throughout the world with quantifiable speed. This virus grew fairly easily in tissue culture, enabling quick sequencing of the genome. Sequencing differed sufficiently from any of the known human or animal coronaviruses to place this virus into a new group, along with a virus that was subsequently cultured from Himalayan palm civets, from which it presumably had emerged.
During the 2002–2003 outbreak, SARS infection was reported in 29 countries in North America, South America, Europe, and Asia. Overall 8098 infected individuals were identified, with 774 SARS-related fatalities. It is still unclear how the virus entered the human population and whether the Himalayan palm civets were the natural reservoir for the virus.
Sequence analysis of the virus isolated from the Himalayan palm civets revealed that this virus contained a 29-nucleotide sequence not found in most human isolates, in particular those involved in the worldwide spread of the epidemic.
In animal viruses, this nucleotide sequence maintains the integrity of the 10th open reading frame (ORF); whereas in the human strains, the absence of this motif results in 2 overlapping ORFs. The function of the ORFs in the animal and human isolates is unknown, and it is unclear whether the deletion of the 29-nucleotide sequence played a role in the trans-species jump, the capacity of the epidemic strain to spread between humans or the virulence of the virus in humans.
Curiously data from seroepidemiologic studies conducted among food market workers in areas where the SARS epidemic likely began indicated that 40% of wild animal traders and 20% of individuals who slaughter animals were seropositive for SARS, although none had a history of SARS-like symptoms.25 These findings suggest that these individuals were exposed through their occupation to a SARS-like virus that frequently caused an asymptomatic infection. Infection control policies may have contributed to the halt of the SARS epidemic.
The last series of documented cases to date, in April 2004, was laboratory-acquired.
The SARS epidemic gave the world of coronaviruses an enormous infusion of energy and activity that contributed to the large amount already known about the virology and parthenogenesis of coronavirus infections from the expanding area of veterinary virology.
Shortly after, Fouchier reported the identification of a coronavirus, named NL, isolated from an 8-month-old boy with pneumonia and grown from a clinical specimen that was obtained in April 1988. Genomic amplification techniques, based on arbitrarily primed reverse transcriptase-polymerase chain reaction (RT-PCR), were used to identify viral sequences. Full genomic sequence analysis of NL showed that this virus was also a group I coronavirus and closely related to NL63.
Four of 139 (2.9%) respiratory specimens collected from November 2000 to January 2002 tested positive for NL.33 Respiratory tract disease was observed in these 4 children whose ages ranged from 3 months to 10 years. The discovery of both NL63 and NL depended on the propagation of the viruses in cell culture.

With the use of molecular probes that targeted conserved regions of the coronavirus genome, months later, Esper et al found evidence of a human respiratory coronavirus in respiratory specimens obtained from children younger than 5 years of age, which was designated the New Haven coronavirus (HCoV-NH). This approach was based on the theory that the gene for the viral replicase of all coronaviruses has conserved genetic sequences that encode indispensable, essential functions and that these sequences could be targeted for virus identification and discovery.
This approach did not require propagation of the virus in cell culture, organ cultures, or experimental animals and could be performed directly on respiratory secretions.
After the initial identification of novel sequences of HCoV-NH, specific probes were used to screen respiratory specimens collected between January 2002 and February 2003 from children younger than 5 years of age whose respiratory specimens tested negative for the respiratory syncytial virus, influenza, parainfluenza, and adenoviruses. Of 895 children, 79 (8.8%) tested positive for HCoV-NH by RT-PCR, a majority of whom were sampled in the winter and spring seasons.
Sequence and phylogenetic analysis based on the replicate gene showed that HCoV-NH was closely related to both NL63 and NL, although the full genomic sequence of HCoV-NH has not been completed. Cough, rhinorrhea, and tachypnea were present in more than one-half of the children infected with HCoV-NH. Eleven children were in the newborn intensive care unit at the time of their sampling and had been hospitalized since birth, suggesting either nosocomial infection or a less likely cause of vertical transmission.
One child, a 6-month-old who tested positive for HCoV-NH, also carried a diagnosis of Kawasaki disease, vasculitis of early childhood. In a subsequent case-control study, 8 of 11 (72.7%) children with Kawasaki disease tested positive for HCoV-NH while only 1 of 22 (4.5%) age- and time-matched controls tested positive for HCoV-NH (P = 0.0015).36 By correlating these findings, Graf37 detected the presence of a peptide corresponding to the spike glycoprotein of NL63, the closely related virus identified in the Netherlands, in tissue from individuals with Kawasaki disease.
The summation of these findings suggests that HCoV-NH may play a role in the pathogenesis of Kawasaki disease. Further research is necessary to determine whether HCoV-NH is the cause of Kawasaki disease.
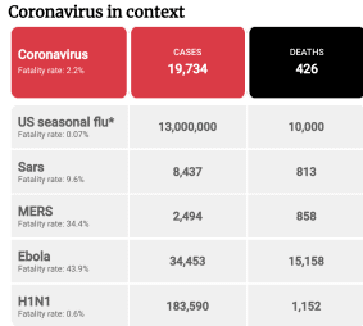
2019 Novel Coronavirus (2019-nCoV) is a virus (more specifically, a coronavirus) identified as the cause of an outbreak of respiratory illness first detected in Wuhan, China. Early on, many of the patients in the outbreak in Wuhan, China reportedly had some link to a large seafood and animal market, suggesting animal-to-person spread. However, a growing number of patients reportedly have not had exposure to animal markets, suggesting person-to-person spread is occurring. At this time, it’s unclear how easily or sustainable this virus is spreading between people. The latest situation summary updates are available on CDC’s web page 2019 Novel Coronavirus, Wuhan, China.
Symptoms
Patients with the confirmed 2019-nCoV infection have reportedly had mild to severe respiratory illness with symptoms of:
fever
cough
shortness of breath
CDC believes at this time that symptoms of 2019-nCoV may appear in as few as 2 days or as long as 14 after exposure. This is based on what has been seen previously as the incubation period of MERS viruses.
Situation Summary
The Centers for Disease Control and Prevention (CDC) is closely monitoring an outbreak of respiratory illness caused by a novel (new) coronavirus first identified in Wuhan, Hubei Province, China. Chinese authorities identified the new coronavirus, which has resulted in hundreds of confirmed cases in China, including cases outside Wuhan, with additional cases being identified in a growing number of countries internationally. The first case in the United States was announced on January 21, 2020.
How it Spreads
Coronaviruses are a large family of viruses that are common in many different species of animals, including camels, cattle, cats, and bats. Rarely, animal coronaviruses can infect people and then spread between people such as MERS and SARS. Many of the patients in the pneumonia outbreak caused by 2019-nCov in Wuhan, China had some link to large seafood and live animal markets suggesting animal-to-person spread. However, a growing number of patients reportedly have not had exposure to animal markets, indicating person-to-person spread is occurring.
When person-to-person spread has occurred with MERS and SARS, it is thought to have happened via respiratory droplets produced when an infected person coughs or sneezes, similar to how influenza and other respiratory pathogens spread. The spread of SARS and MERS between people has generally occurred between close contacts.
It’s important to note that how easily a virus spreads from person to person can vary. Some viruses are highly contagious (like measles), while other viruses are less so. It’s not clear yet how easily 2019-nCoV spreads from person to person. It’s important to know this in order to better understand the risk associated with this virus.
There is much more to learn about the transmissibility, severity, and other features associated with 2019-nCoV, and investigations are ongoing. The latest situation summary updates are available on CDC’s web page 2019 Novel Coronavirus, Wuhan, China.
Prevention & Treatment
There is currently no vaccine to prevent 2019-nCoV infection. The best way to prevent infection is to avoid being exposed to this virus. Right now, 2019-nCoV has not been found to be spreading in the United States, so there are no additional precautions recommended for the general public to take. However, as a reminder, the CDC always recommends everyday preventive actions to help prevent the spread of respiratory viruses, including:
Wash your hands often with soap and water for at least 20 seconds. If soap and water are not available, use an alcohol-based hand sanitizer.
Avoid touching your eyes, nose, and mouth with unwashed hands.
Avoid close contact with people who are sick.
Stay home when you are sick.
Cover your cough or sneeze with a tissue, then throw the tissue in the trash.
Clean and disinfect frequently touched objects and surfaces.
These are everyday habits that can help prevent the spread of several viruses. CDC does have specific guidance for travelers.
Treatment
There is no specific antiviral treatment recommended for 2019-nCoV infection. People infected with 2019-nCoV should receive supportive care to help relieve symptoms. For severe cases, treatment should include care to support vital organ functions.
People who think they may have been exposed to 2019-nCoV should contact their healthcare provider immediately.
See Interim Guidance for Healthcare Professionals for information on patients under investigation.
Second Travel-related Case of 2019 Novel Coronavirus Detected in the United States
Press Release
For Immediate Release: Friday, January 24, 2020
The Centers for Disease Control and Prevention (CDC) today confirmed the second infection with 2019 Novel Coronavirus (2019-nCoV) in the United States has been detected in Illinois. The patient recently returned from Wuhan, China, where an outbreak of respiratory illness caused by this novel coronavirus has been ongoing since December 2019.
The patient returned to the U.S. from Wuhan on January 13, 2020, and called a healthcare provider after experiencing symptoms a few days later. The patient was admitted to a hospital, where infection control measures were taken to reduce the risk of transmission to other individuals. The patient remains hospitalized in an isolation room in a stable condition and is doing well.
Based on the patient’s travel history and symptoms, healthcare professionals suspected 2019-nCoV. A clinical specimen was collected and sent to CDC, where laboratory testing confirmed the infection. The Illinois Department of Public Health (IDPH) and the Chicago Department of Public Health (CDPH) are investigating locations where this patient went after returning to Illinois and are identifying any close contacts who were possibly exposed. The patient has limited close contacts, all of whom are currently well and who will be monitored for symptoms. Since returning from China, the patient has had very limited movement outside the home.
CDC is taking aggressive public health measures to help protect the health of Americans. While the CDC considers this a serious public health threat, based on current information, the immediate health risk from 2019-nCoV to the general American public is considered low at this time. CDC is working closely with the Illinois Department of Public Health, the Chicago Department of Public Health, and other local partners. A CDC team has been deployed to support the ongoing investigation.
However, CDC has been proactively preparing for the introduction of 2019-nCoV in the U.S. for weeks, including:
First alerting clinicians on January 8 to be on the lookout for patients with respiratory symptoms and a history of travel to Wuhan, China.
Developing guidance for clinicians for testing and management of 2019-nCoV, as well as guidance for home care of patients with 2019-nCoV.
Has developed a diagnostic test to detect this virus in clinical specimens. Currently, testing must take place at CDC, but CDC is preparing to share these test kits with domestic and international partners.
Implementing public health entry screening at Atlanta (ATL), Chicago (ORD), Los Angeles (LAX), New York (JFK), and San Francisco (SFO) airports. The CDC is currently evaluating the extent and duration of this enhanced screening.
CDC has activated its Emergency Operations Center to better provide ongoing support.
Coronaviruses are a large family of viruses, some causing respiratory illness in people and others circulating among animals including camels, cats, and bats. Rarely, animal coronaviruses can evolve and infect people and then spread between people, such as has been seen with Severe Acute Respiratory Syndrome (SARS) and Middle East Respiratory Syndrome (MERS). Investigations are ongoing to learn more, but the person-to-person spread of 2019-nCoV is occurring.
It is likely there will be more cases reported in the U.S. in the coming days and weeks. CDC will continue to update the public as circumstances warrant. While the immediate risk of this new virus to the American public is believed to be low at this time, there are simple daily precautions that everyone should always take. It is currently flu and respiratory disease season, and the CDC recommends getting vaccinated, taking everyday preventive actions to stop the spread of germs, and taking flu antivirals if prescribed.
Right now, the CDC recommends travelers avoid all nonessential travel to Wuhan, China. In addition, the CDC recommends people traveling to China practice certain health precautions like avoiding contact with people who are sick and practicing good hand hygiene.
Corona Virus To Reach Pandemic Status. Please click on the video.
The Canadian Press January 27/2020
Ontario confirms second presumptive coronavirus case in the wife of the first patient
TORONTO — Public health officials in Ontario are reporting a second presumptive case of the new coronavirus.
They say the wife of the man who became the first case of the illness in Canada has also tested positive for the virus.
The province says the woman has been in self-isolation since arriving in Toronto with her husband last week.
Chief Medical Officer of health Dr. David Williams said Monday the woman tested positive for the virus at Ontario’s public health laboratory.
“We are working alongside Toronto Public Health, who has been in regular contact with the individual during their self-isolation period,” Williams said in a statement.
China is reporting 2,744 cases and 80 deaths, but it remains to be seen whether the virus is as dangerous as the common flu, which kills thousands every year in Canada alone.
They also say that wearing surgical masks during everyday life has little use in protecting against coronavirus, despite being effective in hospital settings. Early data on the new form of the virus suggest masks won’t be especially effective, and some say that repeatedly touching and adjusting the masks with unwashed hands could do more harm than good.
But the fear that would prompt someone to buy such a mask is perhaps heightened by parallels to the 2002 SARS outbreak that originated in China and infected more than 8,000 people, killing 800. There were 44 Canadians killed by that strain of coronavirus.
This report by The Canadian Press was first published on Jan. 27, 2020.
February 09/2020 Corona Virus update
BEIJING — China’s virus death toll rose by 89 on Sunday to 811, passing the number of fatalities in the 2002-2003 SARS epidemic, but fewer new cases were reported in a possible sign its spread may be slowing as other nations stepped up efforts to block the disease.
Some 2,656 new virus cases were reported in the 24 hours ending at midnight Saturday, most of them in the central province of Hubei, where the first patients fell sick in December. That was down by about 20% from the 3,399 new cases reported in the previous 24-hour period.
“That means the joint control mechanism of different regions and the strict prevention and control measures have worked,” a spokesman for the National Health Commission, Mi Feng, said at a news conference.
Also Sunday, new cases were reported in Japan, South Korea, Vietnam, Malaysia, the U.K., and Spain. More than 360 cases have been confirmed outside mainland China.

March 20 Covid19 Update:
Global Cases:
I personally would recommend a Vitamin B12 Supplement. All year through. Vitamin D3 if you are not getting enough sunshine and Vitamin C for overall health.
Familiarize yourself with these products, and make the decision that suits you best.
If in the event you have to go through a period of isolation make sure you keep up with an exercise of some sort. Yoga is great. Lack of sunshine, get some of that Vitamin3 into you as prescribed.
Also, know you can contact me on my website if you have any questions. Use the comment section and I will reply. I am currently trying to get some coupons going also. This coronavirus storm will subside. Be careful and stay healthy. My site deals with a lot of herbal and home remedies. It is free to use.
Thank you for reading.
Comments are welcome.
Thank you,
Michael
The 2019-ncov is a very bad virus as I have heard alot about it it outbreak but for me I think we all have to be very vare with out dealings especially when it comes to animals and if you know any affected person please report to the relevant and nearest emergency agencies as I would save a life.thamks alot for this awesome article it goods to see someone putting out time to help other.
Hi Feji,
Thank you for your comments.
Best wishes,
Michael
I know that this virus is scary, there are 2 cases now in the States and I hope that it won’t come to NYC. I am planning in traveling in April, hopefully by that time we find the cure or it dies down. I do not know why they all starts in China! Thank you for sharing the facts about this virus.
I used to work in Japan and wearing masks does help and of course personal hygiene will help with this as well. It is best to dispose the mask everyday so you do not get infected.
Stay safe everyone.
Hi Nuttanee,
Thank you for your comments. I hope there is a cure found soon also.
Best wishes,
Michael
I think the SARS CoV deserves even more attention. The epidemic back in 2002 was such a bad experience, especially for the Chinese people. Too bad to the point it took the lives of nearly 10% of those affected by the virus. But thankfully, it was contained. Seeing that it is very easily transmitted, I think we need to tread carefully so a repeat of the last incident don’t happen. Great information. Thanks for sharing.
Hi Rhain,
Thank you for your comments. SARS falls under the umbrella of the corona virus. Coronaviruses were discovered in 1937, unfortunately people have to die before enough is done to protect ourselves.
Best wishes,
Michael
Many thanks to you for sharing such a beautiful article with us, and through you we have learned about the Corona virus and it is a very timely article because the epidemic has now appeared in China. You have described very well through your article how we notice when this virus enters our body. And you also discussed, what should we do if we are infected with this virus. I think since this is a timely topics , everyone will be aware of this after reading your article.
Hi arzu,
Thank you for your comments.
Best wishes,
Michael