What is Dengue Fever
Blue indicates link
I personally had not heard about Dengue Fever, until I started writing an article on the Global Health Risks 2019-2020.
# 1 On The Global Health Risks 2019-2020
Dengue fever is a mosquito-borne tropical disease caused by the dengue virus. Symptoms typically begin three to fourteen days after infection. These may include a high fever, headache, vomiting, muscle and joint pains, and a characteristic skin rash. Recovery generally takes two to seven days. In a small proportion of cases, the disease develops into severe dengue, also known as dengue hemorrhagic fever, resulting in bleeding, low levels of blood platelets, and blood plasma leakage, or into dengue shock syndrome, where dangerously low blood pressure occurs.
It is the fastest-spreading mosquito-borne disease in the world and causes major epidemics in urban areas. The World Health Organization estimates 50 to 100 million cases resulting in 25,000 deaths annually.
Dengue has become a global problem since the Second World War and is common in more than 120 countries, mainly in Asia and South America. About 390 million people are infected a year and approximately 40,000 die. In 2019 a significant increase in the number of cases was seen. The earliest descriptions of an outbreak date from 1779. Its viral cause and spread were understood by the early 20th century. Apart from eliminating the mosquitoes, work is ongoing for medication targeted directly at the virus. It is classified as a neglected tropical disease.
We should be informed especially if we travel to the countries mentioned.
Dengue fever is listed as a global threat in 2019/2020
US States
- 1,203 dengue cases reported
US Territories
- 56 dengue cases reported
On 12 February 2020, the European Centre for Disease Prevention and Control (ECDC) reported an increase in the number of cases of dengue infection in French Guiana, Guadeloupe, Martinique, and Saint-Martin. In January 2020, health authorities in the region declared a dengue epidemic in Guadeloupe and Saint-Martin and indicated that Martinique is also at risk of an epidemic.
Global burden of dengue:
The incidence of dengue has grown dramatically around the world in recent decades. A vast majority of cases are asymptomatic or mild and self-managed, and hence the actual numbers of dengue cases are under-reported. Many cases are also misdiagnosed as other febrile illnesses.
One modeling estimate indicates 390 million dengue virus infections per year (95% credible interval 284–528 million), of which 96 million (67–136 million) manifest clinically (with any severity of disease). Another study on the prevalence of dengue estimates that 3.9 billion people are at risk of infection with dengue viruses. Despite the risk of infection existing in 129 countries, 70% of the actual burden is in Asia.
The number of dengue cases reported to WHO increased over 15fold over the last two decades, from 505,430 cases in 2000 to over 2,400,138 in 2010 and 3,312,040 in 2015. Deaths from 2000 to 2015 increased from 960 to more than 4032.
This alarming increase in case numbers is partly explained by a change in national practices to record and report dengue to the Ministries of Health, and to the WHO. But it also represents government recognition of the burden, and therefore the pertinence to report dengue disease burden. Therefore, although the full global burden of the disease is uncertain, this observed growth only brings us closer to a more accurate estimate of the full extent of the burden.
The largest number of dengue cases ever reported globally was in 2019. All regions were affected, and dengue transmission was recorded in Afghanistan for the first time.
The American region alone reported 3.1 million cases, with more than 25,000 classified as severe. Despite this alarming number of cases, deaths associated with dengue were fewer than in the previous year.
The high number of cases was reported in Bangladesh (101,000), Malaysia (131,000) Philippines (420,000), and Vietnam (320,000) in Asia.
The worldwide incidence of Dengue fever: 50 million worldwide cases
Prevalence of Dengue fever: 100 to 200 cases are reported annually to the U.S. Centers for Disease Control and Prevention (CDC), mostly in people who have recently traveled abroad. (Source: excerpt from Dengue Fever: NIAID) … In 1995, 250,000 cases of DF and 7,000 cases of DHF were reported in the Americas (Source: excerpt from Dengue Fact Sheet: DVBID)
Worldwide prevalence of Dengue fever:
Each year, tens of millions of cases of dengue fever occur and, depending on the year, up to hundreds of thousands of cases of DHF.
What is my risk?
All travelers are at risk in areas where dengue occurs. The risk is higher during the daytime, particularly around sunrise and sunset. Mosquitoes can transmit dengue bite even in shady areas when it is overcast, or if you are indoors. The risk is lower for travelers who stay only a few days in air-conditioned hotels with well-kept grounds and who participate in outdoor activities during non-peak biting periods.
The risk increases for those spending longer periods of time in areas where dengue occurs, including aid and humanitarian workers and/or those who stay in the homes of friends and relatives.
A person who recovers from one of the four types of dengue will have lifelong immunity against that particular type but not against the others.
How is it transmitted?
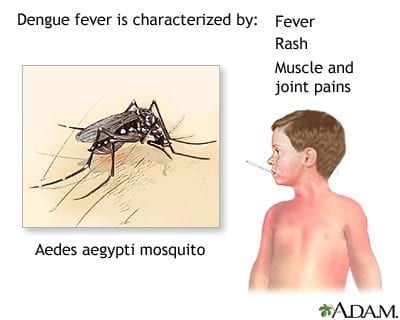
- Dengue fever is spread to humans through the bite of an infected mosquito, particularly the Aedes aegypti and Aedes albopictus species.
- Mosquitoes carrying dengue typically bite during the daytime, particularly around sunrise and sunset. They breed in standing water and are often found in urban and semi-urban areas.
Other modes of transmission:
The primary mode of transmission of DENV between humans involves mosquito vectors. There is evidence, however of the possibility of maternal transmission (from a pregnant mother to her baby). Vertical transmission rates appear low, with the risk of vertical transmission seemingly linked to the timing of the dengue infection during the pregnancy. When a mother does have a DENV infection when she is pregnant, babies may suffer from preterm birth, low birth weight, and fetal distress
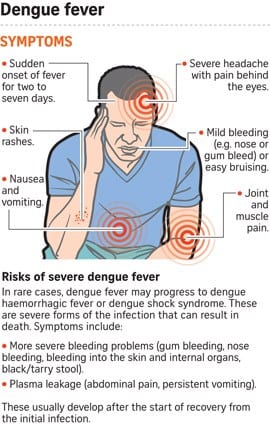
What are the symptoms?
- The symptoms most commonly appear three to fourteen days after being bitten by an infected mosquito.
- They usually include flu-like symptoms such as high fever, severe headache, pain behind the eyes, joint and muscle pain, nausea, vomiting, and a rash.
- It is common for some people to show no symptoms and most people recover from dengue fever after a few days.
- In a small percentage of cases, people with dengue fever develop dengue hemorrhagic fever, also known as severe dengue. Warning signs usually occur three to seven days after the first symptoms, and include a decrease in fever, bleeding from the nose or gums, fatigue, severe abdominal pain, persistent vomiting, and difficulty breathing.
- Children growing up in risk areas are at a higher risk of severe dengue.
- Severe dengue can lead to shock. With proper medical care, almost all cases will survive.
Disease characteristics (signs and symptoms)
Dengue is a severe, flu-like illness that affects infants, young children, and adults, but seldom causes death. Symptoms usually last for 2–7 days, after an incubation period of 4–10 days after the bite from an infected mosquito. The World Health Organization classifies dengue into 2 major categories: dengue (with/without warning signs) and severe dengue. The sub-classification of dengue with or without warning signs is designed to help health practitioners triage patients for hospital admission, ensure close observation, and minimize the risk of developing more severe dengue (see below).
Dengue:
Dengue should be suspected when a high fever (40°C/104°F) is accompanied by 2 of the following symptoms during the febrile phase:
- severe headache
- pain behind the eyes
- Muscle and joint pains
- nausea
- vomiting
- swollen glands
- rash.
Severe dengue:
A patient enters what is called the critical phase normally about 3-7 days after illness onset. It is at this time when the fever is dropping (below 38°C/100°F) in the patient, that warning signs associated with severe dengue can manifest. Severe dengue is a potentially fatal complication, due to plasma leaking, fluid accumulation, respiratory distress, severe bleeding, or organ impairment.
Warning signs that doctors should look for include:
- severe abdominal pain
- persistent vomiting
- rapid breathing
- bleeding gums
- fatigue
- restlessness
- blood in vomit.
If patients manifest these symptoms during the critical phase, close observation for the next 24–48 hours is essential so that proper medical care can be provided, to avoid complications and risk of death.
Diagnostics:
Several methods can be used for the diagnosis of DENV infection. These include virological tests (that directly detect elements of the virus) and serological tests, which detect human-derived immune components that are produced in response to the virus). Depending on the time of patient presentation, the application of different diagnostic methods may be more or less appropriate. Patient samples collected during the first week of illness should be tested by both serological and virological methods (RT-PCR).
Virological methods:
The virus may be isolated from the blood during the first few days of infection. Various reverse transcriptase-polymerase chain reaction (RT–PCR) methods are available. In general, RT–PCR assays are sensitive, but they require specialized equipment and technical training for staff implementing the test, therefore they are not always available in all medical facilities. RT–PCR products from clinical samples may also be used for genotyping of the virus, allowing comparisons with virus samples from various geographical sources.
The virus may also be detected by testing for a virus-produced protein, called NS1. There are commercially produced rapid diagnostic tests available for this because it takes only ~20 minutes to determine the result, and the test does not require specialized laboratory techniques or equipment.
Serological methods:
Serological methods, such as enzyme-linked immunosorbent assays (ELISA), may confirm the presence of a recent or past infection, with the detection of IgM and IgG anti-dengue antibodies. IgM antibodies are detectable ~1 week after infection and are highest at 2 to 4 weeks after the onset of illness. They remain detectable for about 3 months. The presence of IgM is indicative of a recent DENV infection. IgG antibody levels take longer to develop than IgM, but IgG remains in the body for years. The presence of IgG is indicative of a past infection.
Treatment:
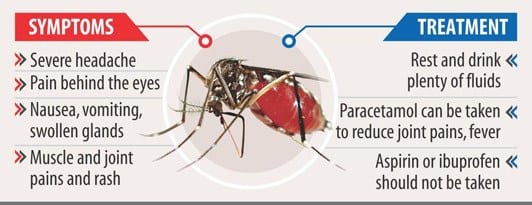
There is no specific treatment for dengue fever.
Fever reducers and painkillers can be taken to control the symptoms of muscle aches and pains, and fever.
- The best options to treat these symptoms are acetaminophen or paracetamol.
- NSAIDs (non-steroidal anti-inflammatory drugs), such as ibuprofen and aspirin should be avoided. These anti-inflammatory drugs act by thinning the blood and is a disease with a risk of hemorrhage, blood thinners may exacerbate the prognosis.
For severe dengue, medical care by physicians and nurses experienced with the effects and progression of the disease can save lives – decreasing mortality rates from more than 20% to less than 1%. Maintenance of the patient’s body fluid volume is critical to severe dengue care. Patients with dengue should seek medical advice upon the appearance of warning signs.
There is no medicine for treating dengue fever. Mild cases may be treated at home with rest and plenty of fluids to prevent dehydration. You may take acetaminophen (Tylenol) for pain. But don’t take anti-inflammatory medicines like aspirin, ibuprofen (such as Advil or Motrin), or naproxen (such as Aleve). They may increase the risk of bleeding. Be safe with medicines. Read and follow all instructions on the label. People with mild cases of dengue fever usually feel better within 2 weeks.
Dengue hemorrhagic fever, the more serious form of dengue fever, usually requires treatment in a hospital. You may need intravenous (IV) fluids to treat dehydration. You also may need a blood transfusion to replace lost blood. You will be closely watched for signs of shock.
Vaccination against dengue:
The first dengue vaccine, Dengvaxia® (CYD-TDV) developed by Sanofi Pasteur was licensed in December 2015 and has now been approved by regulatory authorities in ~20 countries. In November 2017, the results of additional analysis to retrospectively determine serostatus at the time of vaccination were released. The analysis showed that the subset of trial participants who were inferred to be seronegative at the time of first vaccination had a higher risk of more severe dengue and hospitalizations from dengue compared to unvaccinated participants. As such, the use of the vaccine is targeted at persons living in endemic areas, ranging from 9-45 years of age, who have had at least 1 documented dengue virus infection previously.
If you know you have dengue, avoid getting further mosquito bites during the first week of illness. A virus may be circulating in the blood during this time, and therefore you may transmit the virus to new uninfected mosquitoes, who may, in turn, infect other people.
“WHO”, position on the CYD-TDV vaccine:
As described in the WHO position paper on the Dengvaxia vaccine (September 2018) the live attenuated dengue vaccine CYD-TDV has been shown in clinical trials to be efficacious and safe in persons who have had a previous dengue virus infection (seropositive individuals). However, it carries an increased risk of severe dengue in those who experience their first natural dengue infection after vaccination (those who were seronegative at the time of vaccination). For countries considering vaccination as part of their dengue control program, pre-vaccination screening is the recommended strategy.
With this strategy, only persons with evidence of a past dengue infection would be vaccinated (based on an antibody test, or on a documented laboratory-confirmed dengue infection in the past). Decisions about implementing a pre-vaccination screening strategy will require a careful assessment at the country level, including consideration of the sensitivity and specificity of available tests and of local priorities, dengue epidemiology, country-specific dengue hospitalization rates, and affordability of both CYD-TDV and screening tests.
Vaccination should be considered as part of an integrated dengue prevention and control strategy. There is an ongoing need to adhere to other disease prevention measures such as well-executed and sustained vector control. Individuals, whether vaccinated or not, should seek prompt medical care if dengue-like symptoms occur.
Prevention and control:
If you know you have dengue, avoid getting further mosquito bites during the first week of illness. The virus may be circulating in the blood during this time, and therefore you may transmit the virus to new uninfected mosquitoes, who may, in turn, infect other people.
The proximity of mosquito vector breeding sites to human habitation is a significant risk factor for dengue as well as for other diseases that the Aedes mosquito transmits. At present, the main method to control or prevent the transmission of the dengue virus is to combat the mosquito vectors. This is achieved through:
- Prevention of mosquito breeding:
- Preventing mosquitoes from accessing egg-laying habitats by environmental management and modification;
- Disposing of solid waste properly and removing artificial man-made habitats that can hold water;
- Covering, emptying, and cleaning of domestic water storage containers on a weekly basis;
- Applying appropriate insecticides to water storage outdoor containers;
- Personal protection from mosquito bites:
- Use personal household protection measures, such as window screens, repellents, insecticide-treated materials, coils, and vaporizers. These measures must be observed during the day both inside and outside of the home (e.g.: at work/school) because the primary mosquito vectors bite throughout the day;
- Wearing clothing that minimizes skin exposure to mosquitoes is advised;
- Community engagement:
- Educating the community on the risks of mosquito-borne diseases;
- Engaging with the community to improve participation and mobilization for sustained vector control;
- Reactive vector control:
- Emergency vector control measures such as applying insecticides as space spraying during outbreaks may be used by health authorities;
- Active mosquito and virus surveillance:
- Active monitoring and surveillance of vector abundance and species composition should be carried out to determine the effectiveness of control interventions;
Can dengue fever be treated?
There is no specific treatment for dengue fever but medical care can help with recovery and the control of symptoms.
Where is dengue fever a concern?
- Dengue fever is found throughout the world but mainly occurs in tropical and subtropical areas.
- It is widespread in regions of Africa, Central and South America, the Caribbean, the Eastern Mediterranean, South and Southeast Asia, and Oceania.
- The World Health Organization (WHO) estimates that over 40% of the world’s population lives in areas where dengue viruses can be transmitted.
Recommendations:
Consult a health care provider or visit a travel health clinic preferably six weeks before you travel.
- Protect yourself from mosquito bites, particularly around sunrise and sunset.
- If you develop symptoms similar to dengue fever when you are traveling or after you return, see a healthcare provider and tell them where you have been traveling or living.
The overall incidence of dengue, as well as the explosive outbreaks of dengue, has been increasing dramatically over the last several years. Older data suggested an estimated 50-100 million cases of dengue fever and 500,000 cases of dengue hemorrhagic fever occur worldwide, with 22,000 deaths (mainly in children).
In 2015, official data from WHO member states reported more than 3.2 million cases, with 2.35 million cases in the Americas alone, including 10,200 cases of severe dengue and 1181 deaths.
One study estimates that approximately 390 million dengue infections occur per year (95% CI; 284-528 million), with 96 million of these presenting clinically. An estimated 2.5-3 billion people (approximately 40%-50% of the world’s population) are estimated to be at risk for dengue infection. Recent
estimates find that 128 countries worldwide are at risk for dengue infection, which includes 36 that had once been classified as dengue-free. The only continent that has not experienced dengue transmission is Antarctica.
Other Interesting Facts I Found:
About 50% of the world’s population lives under the threat of dengue, which is responsible for approximately 390 million infections globally per year.
Before 1970, only nine countries had experienced severe dengue epidemics. The disease is now endemic in more than 100 countries.
In the USA, the US Centers for Disease Control (CDC) confirmed 865 travel-related Dengue cases in 2019 and issued a Level 1 Travel Alert on October 2, 2019, related to the Dengue outbreak in the Americas. In the state of Florida, a 2nd Alert was issued by the Department of Health in October 2019.
Is There A Dengue Vaccine?
One dengue vaccine, Dengvaxia has been approved for use in some countries. But, it is not yet available in Canada. This dengue vaccine has proven effective in tests conducted in Asia and Latin America.
Dengue Virus Vaccine:
Dengue virus, with high morbidity and mortality rates, is a single positive-stranded RNA virus that often occurs in tropical and subtropical regions. Dengue virus has caused millions of infections each year. Studies conducted on the dengue virus indicate that it is associated with a wide variety of diseases, including dengue hemorrhagic fever and dengue shock syndrome. The dengue virus vaccine has been widely used in various dengue virus-related disease prevention. Several recombinant live-attenuated dengue vaccines have shown no adverse effects and high safety in the clinic.
WHY HAVE CASES SPIKED THIS YEAR?
Once confined mostly to cities in tropical climates, dengue is now found in at least 125 countries across the world, with around 100 million infected every year and some four billion people living in dengue-prone areas, according to the journal Nature Microbiology.
The disease is cyclical — dramatic outbreaks occur every few years — but climate change is believed to have contributed to a spike in cases in 2019, with July clocked as the warmest on record.
“Extremely warm temperatures we’ve seen this year” likely facilitated its spread, Rachel Lowe, assistant professor at the London School of Hygiene & Tropical Medicine, told AFP since mosquitoes thrive in warm weather climates.
Several European countries where dengue was once marginal have seen outbreaks, while Latin American countries including Brazil, Colombia, Honduras, and Nicaragua are tackling a surge in cases.
Dengue Vaccine in the United States:
In May 2019, Dengvaxia® was approved external icon by the U.S. Food and Drug Administration (FDA) in the United States for use in children 9-16 years old living in an area where dengue is common (the U.S. territories of American Samoa, Puerto Rico, and the US Virgin Islands), with laboratory-confirmed prior dengue virus infection.
Information on the vaccine’s availability in the US territories is pending.
Side Effects:
Common side effects include headache, pain at the site of injection, and general muscle pains. Severe side effects may include anaphylaxis. Use is not recommended in people with poor immune function. The safety of use during pregnancy is unclear. Dengvaxia is a weakened but live vaccine and works by triggering an immune response against four types of dengue virus.
As of 2016, the dengue vaccine had been approved for medical use in eleven countries and in 2019, was approved for medical use in the United States. It is on the World Health Organization’s List of Essential Medicines, the safest and most effective medicines needed in a health system. In Indonesia, it costs about US$207 for the recommended three doses as of 2016. The development of dengue vaccines began in the 1920s but was hindered by the need to create immunity against all four dengue stereotypes. Several other vaccine candidates are in development including live attenuated, inactivated, DNA, and subunit vaccines.
Personal Note:
I am really sorry to hear that the only vaccine against dengue fever is not available in all countries. Also, hearing about the side effects scares me. In certain parts of the Philippines, I hear it is being recalled.
Do more people have to die before, something significant is done? Being aware and informed are your best defenses.
Let us not let this be another, “Corona Virus”.
Thank you for reading,
Michael.
Comments are welcome
Hello Michael, I must say that this article is very helpful and informative. I heard about this disease recently and I decided to do a research on it as I am afraid that my father has similar symptoms. It is great I stumbled upon your article because you explained everything well, now I can consult with my doctor.
Hi Danijel,
Thank you for your comments. Please if you have any doubts about your father, have him diagnosed right away. There is no cure for dengue fever. Early diagnosis is the only cure. I am not sure where you live, but if you live in a country with warm temperatures, and there are mosquitoes flying around, it is better to be safe than sorry. I wish your father good health.
All the best,
Michael
Michael, I truly did not know something like Dengue Fever even exists. What was quite shocking to me is that a mosquito-borne disease caused by a virus of the same name- I thought that you only get yellow-fever and malaria from mosquitos. The number of reported cases are very high. Tell me, does this occur in South Africa as well? It makes me wonder as you stated here: Let us not let this be another, “Corona Virus”.—- Is Social Media hammering on something that is a scare tactic to control the masses? If I look at the statistics you post here this Dengue Fever can be as violent and get out of control like the Corona Virus- Makes me wonder.
Are people’s focus points on the wrong fever?
Hi Karen,
Thank you for your comments. I could not find any recent statics related to South Africa. Here is what I found:
It is the fastest-spreading mosquito-borne disease in the world and causes major epidemics in urban areas. The World Health Organization estimates 50 to 100 million cases resulting in 25,000 deaths annually.
In South Africa, a confirmed dengue outbreak with local transmission occurred in Durban, KwaZulu-Natal Province, in the summer of 1926/27.6,7 During the past twenty-five years sporadic cases of dengue have been reported in South Africa. I am sure the numbers are higher today as there is only one vaccine, and that is very controversial. No treatment since 1926, there is something wrong here.
Best wishes,
Michael
Hello,
Oh! thanks to you for sharing this article with us, too much relevant with nowadays. Like a Corona virus which is most alarming issue in whole world. But I never thought that Dengue fever also can damage person like this! Also there is no vaccine against Dengue fever! And it’s side effects makes me feel scared like Corona virus. I think we should be more concern about it also from your article people can know about it well. Good content you’ve been chosen!
Hi Hmilmee,
Thank you for your comments. Dengue fever is deadly. There is a controversial vaccine out there, but there is no cure. This disease came out after World War 2. I think there is something wrong here.
All the best,
Michael
Thank you so much for sharing with us such a beautiful article with educational tips about TREATMENT DENGUE FEVER.
It is not only the remedies that you have suggested here that are of interest and help but also the context that you offer in the first part of the post. it is clear to find a plain-speaking piece that clarifies what it, in which it has come from, the way it has developed and what to expect and I learned a lot by reading your article. I think this article will benefit everyone. Thanks for sharing a useful and informative post.Thanks
Hi sabrinamou,
Thank you for your comments. What is sad is that Dengue Fever came out after world war 2 and they still do not have a reliable vaccine for it. There also is no real treatment for it.
All the best,
Michael